Sinusitis due to tooth pain is far from a rare occurrence. Doctors even distinguish a separate type of this disease - odontogenic sinusitis, that is, caused by inflammation and infection mainly in the roots of the teeth. Why does this happen? How to deal with this? And can, on the contrary, teeth hurt with sinusitis?
From the point of view of anatomy and physiology, it is not surprising that an infection from a tooth easily passes into the maxillary sinus and vice versa. Despite the fact that there is an anatomical barrier between them, it is very easy to overcome. Violation of its integrity can occur either through the fault of the patient or as a result of unqualified actions on the part of the dentist. However, when answering the question of whether it is necessary to treat teeth for sinusitis, doctors unequivocally say yes. But only with a competent specialist under the supervision of a radiovisiograph or x-ray. Dental treatment is best done outside the acute phase, however, in advanced cases, urgent surgical intervention may be indicated.
Structural features
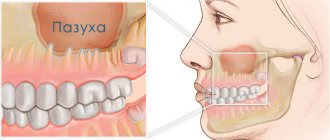
The maxillary (maxillary, main) sinus is located inside the bone of the upper jaw. It is delimited from the oral cavity by the alveolar process. It forms the bottom of the cavity. The volume of the cavity of the upper jaw can be up to ten cubic centimeters. She has a communication with the nasal cavity. The inside of the cavity is lined with mucous tissue.
The structure has features that make it easy to damage:
- Sometimes the thickness of the bone plate between the bottom of the cavity and the roots of the teeth does not exceed one millimeter.
- There is a variant of the location of the roots of the second and first molars, when they penetrate into the cavity and are delimited from it only by the mucous membrane that lines the sinuses.
- The bone plate quickly thins out during inflammatory processes.
- Small thickness of trabeculae of the upper jaw bone.
Such structural features cause slight damage to its wall, even when the doctor did not violate any rules and did not apply significant force.
Rehabilitation after maxillary sinusotomy
In the period after surgery, the patient may need tamponade on the operated side for 8-24 hours. After endoscopic maxillary sinusotomy, it is enough to take painkillers according to the regimen prescribed by the attending physician.
It is necessary to maintain oral hygiene: brush your teeth, gargle with antiseptics and follow all consultations with your doctor.
After studying the reviews about sinusotomy, you can understand whether maxillary sinusotomy is right for you. The price depends on the choice of operation.
What is perforation of the maxillary sinus?
The formation of a defect in the maxillary sinus is a complication during manipulations on the upper jaw. A hole is formed between the oral cavity and the main sinus. This can happen when removing the molars of the upper jaw (molars and premolars) or during prosthetics. And also for complex endodontic treatment of tooth roots and removal of cystic formations. The defect is formed at the site of the tooth socket.
Frequent cases
Perforations of the maxillary sinus occur, as a rule, as a result of the dentist’s work during dental treatment. Tissue ruptures are typical for the following situations:
- Tooth extraction.
- Dental implantation.
- Endodontic therapy.
- Tooth root resection.
If perforation occurred during a tooth extraction operation, this may be a consequence of unskilled and excessively rough work of the dentist, as well as the individual characteristics of the structure of the maxillary sinus of the patient himself. If the dental roots are located directly in the sinus cavity, perforations during the removal of molars are almost inevitable.
One of the complications during endodontic therapy can also be perforation of the tooth root, which in most cases is associated with perforation of the sinus floor. This situation can occur as a result of excessive expansion of the root canals, as well as when using brute force when installing pins and compacting cement for fillings. In this case, most often not only the root of the tooth may be in the maxillary sinus, but also its fragments and particles of filling material. And this is dangerous for the patient.
When a rupture occurs during installation of an implant or during filling a root canal, as well as as a result of inserting pins into the root of a tooth, this in the vast majority of cases is a therapeutic error by a specialist. Sometimes you can find the roots of a wisdom tooth in the maxillary sinus.
Causes of perforation.
The dentist is not always to blame for this complication. It can often appear due to the individual anatomical characteristics of the patient. It may also be due to the course of the inflammatory process in the tissue surrounding the root.
The causes of perforation may be the following:
- Perforation of the maxillary sinus during tooth extraction occurs most often. Its bottom is perforated when a tooth is suddenly removed with great force.
- In some patients, the roots of the upper teeth penetrate into the sinus cavity. When teeth are removed, the integrity of the bone plate is automatically violated. During treatment, filling material may enter the cavity.
- For technically complex endodontic treatment. With this type of treatment, the inflammatory focus is located deep in the gums or under the root of the tooth. Instead of removing the diseased tooth, the dentist tries to save it. During this type of treatment, the bone plate is easily damaged.
- In the process of installing an implant in the upper jaw bone with subsequent dental prosthetics, the maxillary cavity can be easily damaged. This is because the implant is similar to a screw and must be screwed into the bone. If there are defects in this manipulation or anatomical and topographical features, the patient’s bone plate of the upper jaw may be damaged (the size of the implant was incorrectly selected, there were defects in preparation for implantation). Before placing an implant, the doctor does not take into account the fact that when a tooth is removed, the thickness of the bone plate quickly decreases.
- Perforation can occur due to chronic inflammation of the tissues surrounding the tooth (periodontitis). With this pathology, the bone plate delaminates and becomes thin. If a tooth has to be removed in such a situation, perforation almost always occurs.
- Carrying out manipulation to remove an impacted tooth from the maxillary cavity.
- Perforation often occurs during tooth root resection procedures. The need for this manipulation arises when extracting a root with a festering cyst.
Odontogenic sinusitis is a disease that is in the area of interest of two medical specialties - otorhinolaryngology and dentistry, which raises problems in the treatment tactics of patients. Every otorhinolaryngologist encounters odontogenic sinusitis in his practice. To date, despite significant progress in the treatment of pathology of the dental system, the number of patients with odontogenic sinusitis not only does not decrease, but is also steadily growing [6]. According to statistics, the frequency of identification of patients with odontogenic sinusitis ranges from 3 to 25% among patients in otorhinolaryngological and dental medical institutions [5].
According to the classification of A.V. Buskina and V.Kh. Gerber [1], odontogenic maxillary sinusitis is divided into:
- Perforated. As a result of tooth extraction, communication between the maxillary sinus and the oral cavity occurs and an inflammatory process develops.
- Imperforate. Call:
- carious teeth of the upper jaw and chronic periodontitis of large and small molars of the upper jaw;
- hilar cysts and granulomas;
- periodontal disease;
foreign bodies of the maxillary sinus (filling material, tooth root, including dystopic and impacted).
An impacted tooth is quite rare in practice. Tooth retention is an anomaly in the development of the dental system, in which a normally or abnormally developed tooth did not erupt at the appropriate time in a strictly defined place in the alveolar process. In cases where the tooth moves significantly, occupying an abnormal position, and can erupt into the maxillary sinus, nasal cavity, or orbit, such a pathological process is called dystopia. The combination of retention and dystopia is called a “lost” tooth [4]. Retention with dystopia can be observed with both primary and permanent teeth; permanent teeth can be complete or supernumerary. The presence of an impacted tooth in the cavity of the maxillary sinus is very rare and is often discovered by chance. Even less often, a “lost” supernumerary tooth is found in the cavity of the maxillary sinus.
Considering the practical significance and lack of literary publications on this topic, we considered it necessary to share our observation. Its distinctive feature is the so-called odontogenic form of sinusitis observed by us, identified by a number of authors [2]. The most common cause of the odontogenic form is foreign bodies of the maxillary sinus. In such patients, anatomical changes in the nasal cavity (deviated nasal septum, turbinate hypertrophy, nasal polyps, etc.), disrupting its architectonics, aggravate the course of odontogenic sinusitis and become a component of the pathogenesis of the inflammatory process. With odontogenic sinusitis, there are changes in all the walls of the maxillary sinus with thickening or polypous changes in the mucous membrane, in contrast to odontogenic sinusitis, in which there are mainly changes in the lower and anterior walls and, to a lesser extent, the inflammatory process spreads to other paranasal sinuses. The peculiarity of our observation is that the patient had anatomical defects in the structure of the ostiomeatal complex and bone deformation of the walls of the maxillary sinus (Fig. 1).
Figure 1. Computed tomography, coronal view.
An ectopic tooth and a bone spine above it. Displacement of the lateral wall of the middle meatus and middle concha. Large bulla aetmoidalis.
Hyperplasia of the mucous membrane of the maxillary sinus and ethmoidal labyrinth.
Patient L., 30 years old, initially had no complaints from the ENT organs. In February 2012, the patient consulted a dentist due to an inflammatory process in the gum area of the upper jaw on the right. During an X-ray examination, in the projection of large molars on the right in the upper jaw in the area of the maxillary sinus, an impacted and dystopic third large molar is visualized. The patient was recommended to consult an otolaryngologist, and treatment was prescribed - rinsing the mouth with a solution of baking soda. Due to the fact that the patient was breastfeeding, systemic antibacterial drugs were not prescribed. Within a few days, positive dynamics were noted. In June 2012, the patient noted mucous discharge from the nose. For 10 days I independently used vasoconstrictor drops and washed my nose with saline solutions without any positive dynamics. The patient began to notice a severe headache, general weakness, malaise, and mucopurulent nasal discharge, and therefore consulted an otolaryngologist. A diagnosis was made: acute maxillary sinusitis; Treatment was prescribed: nasal rinsing with saline solutions, nasal spray Isofra, Erespal, a course of systemic antibiotic therapy (Flemoxin Solutab). During the week, positive dynamics were noted. In July 2012, the patient began to experience discomfort in the right eye, nasal discharge, and pain in the forehead. Conservative treatment was prescribed, after which the patient noted the absence of pain, but nasal discharge and pus draining down the back wall of the throat remained. Upon repeated consultation with the otorhinolaryngologist, a computed tomogram of the paranasal sinuses was recommended. A series of computed tomograms of the paranasal sinuses revealed darkening of the maxillary, frontal, and ethmoid sinuses on the right. In the maxillary sinus on the right, an impacted and dystopic third large molar is visualized, above which a bone spike from the lateral wall of the maxillary sinus is found, which divides the sinus into 2 floors and touches the medial wall of the sinus. The tooth is adjacent to the posterior wall of the maxillary sinus, where a bone defect is visualized (Fig. 2).
Figure 2. Computed tomography of the ED, coronal and axial views. Total darkening of the right maxillary sinus, as well as the cells of the ethmoidal labyrinth on the right. The axial projection sections show that the tooth is located in the posterior wall of the right maxillary sinus.
The patient was recommended for planned surgical treatment, and therefore on December 3, 2012 she was hospitalized in the ENT department of the Central Clinical Hospital of Civil Aviation. At the time of hospitalization, the patient was bothered by mucopurulent nasal discharge, drainage of pus down the back wall of the pharynx, difficulty in nasal breathing, and discomfort in the projection of the right maxillary sinus. The patient was examined on an outpatient basis and prepared for planned surgery. There is no allergic history.
The general condition on admission was satisfactory. The shape of the nose is correct, palpation is painless, the vestibule of the nose is not changed. Nasal breathing is difficult, more on the right, the sense of smell is preserved. The nasal septum is slightly curved to the left in the form of a ridge. The inferior turbinates are swollen and do not contract after anemization. The nasal passages are narrowed, the mucous membrane is moderately hyperemic and moist. During an endoscopic examination of the nose and nasopharynx, a path of pus is visualized from the posterior end of the middle turbinate on the right. The mucous membrane of the oral cavity is pale pink, the tongue is clean and moist. The soft palate is mobile and symmetrical. The oral cavity has been sanitized. The palatine tonsils are unchanged, the lacunae and surfaces of the tonsils are without any features. The vocal folds are gray and close completely during phonation. The eardrums are gray, the identification marks are clear.
On December 4, 2012, under endotracheal anesthesia, the right half of the nose was examined with a 0-degree endoscope. The following are visualized: hypertrophied inferior turbinate; the middle nasal concha, the anterior end of which is polypous. The middle turbinate is displaced laterally. The mucous membrane of the uncinate process is sharply hypertrophied. The natural anastomosis is not visualized. When probing the lateral wall of the nasal cavity with a curved spoon under pressure, pus of a creamy consistency was released. The lower edge of the uncinate process was removed using a reverse punch. In the area of the anastomosis of the maxillary sinus on the right, polypous tissue is visualized (sent for histological examination). Using Blakesley forceps and a shaver, the maxillary sinus anastomosis on the right was expanded. When inserted into the maxillary sinus, the curved shaver head encounters a dense obstruction. The anterior cells of the ethmoidal labyrinth on the right were opened using a shaver. There are no bone bridges between the cells. The frontal pocket is expanded. When viewing the maxillary sinus with a 0- and 30-degree endoscope, the polyposis-changed mucous membrane filling the entire sinus cavity is visualized; when probing with suction from the area of the natural anastomosis to the posterolateral wall of the sinus, the formation of bone density is felt. In the area of the canine fossa on the right, a vertical incision was made in the mucous membrane to the bone, then access to the right maxillary sinus was made using a bur. The sinus cavity is filled with polyposis-altered mucous membrane, pus, and thick mucus. The polypous-altered mucous membrane was removed with a shaver, after which a bone formation in the form of a bone spike became visible, which divides the sinus into two floors. Both floors are filled with polyps and pus. Using a chisel, the formation is separated from the walls of the sinus and removed. On the lower wall of the maxillary sinus, the crown of the dystopic and impacted third large molar became visible. The tooth was removed using Blakesley forceps and a bone spoon (Fig. 3).
Figure 3. Extracted ectopic tooth and bone spine.
A bone defect is visualized in the posterior wall area. A graft was formed from the removed fragment of the bone spike using a bur and placed on the defect of the posterior wall of the maxillary sinus, covered with a biomembrane. The sinus cavity is filled with fragments of the absorbable sponge “Nazopor”.
Shaver removed the hypertrophied posterior ends of the inferior turbinates on both sides.
A submucosal vasotomy of the inferior turbinates was performed using a scalpel and a suction-raspator. Anterior nasal tamponade with elastic tampons.
The postoperative period was uneventful. In order to resolve the infiltrate in the area of the anterior wall of the maxillary sinus, ointment applications with Traumeel S ointment were prescribed. A nasal shower and double toilet of the nasal cavity were performed daily using therapeutic endoscopy. The maxillary sinus was not washed, since after the operation the entire sinus was filled with an absorbable Nasopor sponge, which avoids the accumulation of blood clots in the postoperative period. A blood clot in the maxillary sinus in the postoperative period after endoscopic maxillary sinus brings the following problems: discomfort, heaviness in the area of the sinus projection, fever, and the possibility of bacterial inflammation. The accumulation of a blood clot in the maxillary sinus occurs due to the higher location of its natural anastomosis in relation to the bottom. Typically, FESS surgeons irrigate the operated maxillary sinuses 1 or 2 times. In our case, we used modern, expensive material, which allowed us not to rinse the postoperative cavity, since this was not necessary. The patient has no pain syndrome. Nasal breathing has been restored. The patient was discharged after surgery on the 3rd day in satisfactory condition. During outpatient observation, careful care was taken for the enlarged natural anastomosis of the maxillary sinus using therapeutic endoscopy. The patient quickly recovered and returned to her normal lifestyle.
The use of a combined approach to the maxillary sinus (through its anterior wall and natural anastomosis) provides great opportunities for a surgeon who knows the FESS technology in the surgical treatment of odontogenic sinusitis, including in situations involving impacted teeth.
Symptoms of perforation of the maxillary sinus
How does perforation of the maxillary sinus manifest itself? There are specific symptoms when this happens.
Signs of perforation:
- Bleeding from the tooth socket with the inclusion of air bubbles. When you exhale through the nose, the number of bubbles will increase.
- With perforation, bleeding occurs not only from the tooth socket. It may come from the nasal passage, which is close to the sinus.
- The patient speaks “in his nose” or nasally.
- Then there is a feeling of free passage of air through the tooth socket.
- The patient sometimes notes distension and a feeling of heaviness in the middle third of the face on the affected side.
If the perforation was not recognized immediately and treatment was not carried out, then the symptoms of sinusitis are added to the previous clinic.
Sinusitis manifests itself:
- Body temperature rises.
- The feeling of fullness in the projection of the maxillary sinus intensifies.
- Nasal breathing is difficult.
- The nasal mucosa on the affected side is swollen.
- General weakness increases.
- Aching pain in the nasal region.
- Purulent discharge from the nasal passage on the side where the manipulation took place.
Solution
After a consultation of dentists (surgeon, orthopedist and therapist), the following treatment plan was adopted:
- removal of the entire prosthetic structure (!), removal of 14, 26, 27 teeth with elimination of the infectious focus.
- in the second stage (approximately a month later) bone grafting in the area of the formed defect
- the third stage (approximately after 3 months) is the implantation of artificial roots in place of teeth 24, 25, 26, 27
- after another 3 months, installation of crowns on these implants.
During this period, the patient will wear a temporary prosthesis to replace missing teeth and undergo therapeutic tooth-preserving treatment of teeth 37, 47, 13.
After presenting this information, the entire team of doctors was present at a very sad scene - an adult respectable man, almost crying, talked about the fact that just 2 years ago, for three months, he was treating his teeth, spent 120 thousand rubles on 15 crowns, and now it turned out that his problem has not only not been solved, but has also worsened and requires new physical and moral efforts and new financial costs. After the first shock passed, he asked us a fair question: why did such complications arise?
Methods for determining perforation
This pathology can be identified only on the basis of a characteristic clinic. If there is any doubt, a full range of diagnostic procedures is performed, including instrumental methods.
To diagnose a bone plate defect and subsequently eliminate it, it is necessary to perform the following manipulations when examining the patient:
- Carefully examine the tooth socket after the tooth root has been removed.
- Perform sounding of its bottom.
- Ask the patient to pinch their nose and exhale through the nose. The air will escape into the mouth through the tooth socket.
- If the patient puffs out his cheeks, air passes into the nasal cavity. But this technique can provoke sinus inflammation and should not be used frequently.
Instrumental diagnostic methods include:
- probing the dental and perforation canal using a thin probe;
- CT scan;
- radiography, in the pictures you can see the defect and foreign bodies;
- general blood analysis.
Diagnostics
Diagnosis of perforation of the floor of the maxillary sinus during tooth extraction is based on a typical clinical picture. In doubtful cases, as well as when such a complication is suspected during implantation or endodontic manipulations, it is necessary to use instrumental diagnostic methods:
- Probing the socket of an extracted tooth or perforated canal with a thin probe . This allows us to determine that there is no bone bottom in the wound. In this case, the instrument passes freely through soft tissues and does not encounter obstacles along its path.
- X-ray of the sinus area . In this case, the pictures can reveal both darkening of the cavity due to the accumulation of blood in it, as well as fragments of dental roots, implants or filling material. Sometimes it is advisable to conduct radiography with contrast, when a contrast agent is introduced into the cavity through a perforation fistula.
- Computed tomography , which allows you to determine perforations and the presence of foreign bodies in the sinus with maximum accuracy.
- If old perforations are suspected, general clinical blood tests , the result of which may indicate the presence of an active source of infection in the body.
Treatment of sinus perforation during tooth extraction
The tactics for managing a patient with perforation depends primarily on the condition of the sinus itself and the time of detection of this defect. This defect should only be treated by a qualified specialist.
Treatment of perforation of the main sinus of the upper jaw has the following objectives:
- Closing the defect.
- Prevent the process of inflammation in the sinus.
- Prescribe treatment if there is inflammation.
- If there are foreign particles, they must be removed.
If the perforation was immediately noticed and there are no signs of infection, then the treatment measures are as follows:
- Preservation of a blood clot in a tooth socket.
- Take measures to prevent its infection (application of a tampon with iodine solution).
- Apply stitches to the gums, if necessary.
- Treatment is carried out until the granulations grow and the defect is closed.
- The tampon is not removed from the hole.
- If the defect does not close on its own, it is covered with a plastic plate. It is fixed to the teeth.
- Prescribing a course of drug therapy aimed at counteracting inflammation.
If the perforation is complicated by gum rupture and penetration of foreign particles into the soft tissues surrounding the tooth socket, plastic closure of the defect is performed on the same day. Or after some time, when you are confident that the fabric will hold the seams. Before this, all foreign bodies are removed and areas that have undergone necrosis are excised. The manipulation is performed under x-ray control to make sure that there is no foreign body. If penetration of a foreign body into the cavity occurs, then it is necessary to perform surgery in a hospital setting.
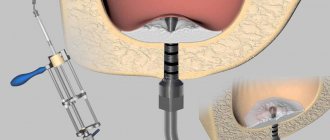
Operation stages:
- Opening of the main sinus of the upper jaw.
- Removal of a tooth from the maxillary sinus (its fragments) and other foreign bodies.
- Excision of necrotic areas.
- Closing the defect.
How we treat
Treatment is carried out only comprehensively and strives to be carried out in one visit , simultaneously:
- Hygienic cleaning and dental treatment We prepare the oral cavity for sterile surgical work. We treat compromised roots. Operations are performed only in a sanitized oral cavity to avoid re-infection.
- The operation is carried out in the surgical department, subject to all conditions of sterile operating rooms. Ultrasound removes inflammatory processes, removes roots that provoked or supported inflammation, eliminates all inflammatory elements, removes cysts, polyps, mucoceles, and foreign bodies.
- Orthopedics Temporary crowns or any other orthopedic elements are fixed to mask the work performed. We do everything to avoid sending the patient home without teeth!
We do not welcome radical and punitive surgery!
Rest assured that after surgery we will never keep you in the hospital unless absolutely necessary.
Levin Dmitry Valerievich Chief physician and founder of the Doctor Levin center
Consequences of perforation of the maxillary sinuses
If the presence of a defect is not noticed and the patient, despite the symptoms, does not consult a doctor, this threatens the onset of serious and dangerous consequences for health.
Possible consequences:
- Severe inflammatory reaction.
- Formation of osteomyelitis.
- Generalization of infection.
- Development of abscess and phlegmon.
- Loss of healthy teeth in the fistula area.
- Chronic sinusitis.
- Meningitis.
- Encephalitis.
- Cavernous sinus thrombosis.
To avoid the formation of complications, the patient should visit the dentist in case of any problems after tooth extraction.
Possible complications
Since inflammation of the maxillary sinuses due to teeth occurs very often, with perforation the symptoms increase significantly.
- After the removal of the upper tooth, sinusitis develops, and then osteomyelitis of the upper jaw.
- The inflammation spreads to other sinuses and paranasal sinuses.
- Teeth located in the perforation zone begin to loosen and fall out.
- A systemic infection develops. The formation of phlegmon and abscesses is possible. Meningitis and meningoencephalitis cannot be excluded.
In case of perforation of the bottom of the maxillary sinus, self-medication is unacceptable. You need to see a doctor as soon as possible!
Old sinus perforation
If the defect is not detected and eliminated in a timely manner, acute inflammation will subside. Within a month, the patient develops a fistula. It connects the gum surface and the sinus cavity. Signs of a chronic inflammatory process appear. This will be a serious complication.
The patient has complaints:
- The presence of dull pain in the upper part of the cheek, of a constant nature. They radiate to the eye area and temporal region.
- Feeling of nasal congestion on one side.
- Separation of pus from the nose and from the fistula on the upper jaw.
- Swelling of the middle third of the face on the affected side.
- Air movement through the defect.
- Difficulty speaking.
- Getting fluid from the mouth into the nose.
Therapy of old processes is associated with significant difficulties. Patients are indicated for surgical treatment in a hospital.
Operation stages:
- Opening of the main sinus of the upper jaw.
- Removing foreign bodies.
- Excision of necrotic areas and granulations.
- Excision of tissues forming the fistula.
- Closing the defect.
After the operation, drug therapy with the use of antibiotics, anti-inflammatory and decongestant drugs is mandatory for a course of two weeks.
Classification and manifestations of pathology
According to the duration of the disease:
- acute - no more than three weeks;
- subacute - duration of illness up to 6 weeks;
- chronic - the disease lasts more than 6 weeks.
Depending on the location of the inflammation:
- pathology on the left;
- pathology on the right;
- bilateral pathology.
When pathology develops due to an extracted tooth, unilateral sinusitis most often develops, but if left untreated, the infection can spread to both sides.
In any case, the disease manifests itself with the same symptoms, but in acute pathology they are more pronounced:
- nasal congestion;
- profuse mucous or purulent runny nose;
- pain from the extracted tooth (localized in the cheek or under the eye);
- throbbing headache;
- pain when tapping on the cheekbones;
- fever;
- general intoxication syndrome - fever, chills, weakness
A distinctive feature of odontogenic sinusitis is its connection with previous dental procedures.
Advantages of treatment in our clinic
Summing up, we can understand that it is very easy to get a septal defect in the cavity of the upper jaw. This depends both on the actions of the dentist and on the individual anatomical characteristics of the patient.
When seeking treatment at our clinic in Moscow, you can be sure that you are guaranteed not to have such complications. We prevent complications.
To do this, we prescribe a mandatory set of preventive measures to prevent them:
- We conduct a complete examination of patients before performing any dental procedures.
- We perform a comprehensive assessment of the patient’s anatomical and topographical features.
- We follow all stages of dental procedures.
You will be satisfied with the quality of dental services if you contact us at the clinic. Our clinic has the most modern equipment at the level of the standards of the best European and American dental clinics. We can offer you a full range of all diagnostic procedures in one place. Our doctors have been trained in the world's leading dental centers and are proficient in the latest treatment and prosthetic techniques. We will help even in the most difficult cases. We develop an individual course of treatment taking into account all the characteristics of the patient. We use only proven treatment methods and materials of the highest quality. Our clinic has made the highest quality dental services available. You can view the full range of our treatment and diagnostic capabilities on our website.
Preventive actions
Prevention of perforations of the floor of the maxillary sinus consists of:
- in a full examination of the patient before complex dental procedures;
- in the correct assessment of the anatomical and topographical characteristics of each person;
- in strict adherence to the technology of therapeutic manipulations.
Timely detection of signs of perforation and its adequate treatment is the key to a favorable outcome for the patient. Incorrect therapeutic tactics or self-medication can aggravate the course of such a complication and cause the development of severe negative consequences.
Features of the maxillary sinus
The maxillary, or maxillary, sinus is a cavity inside the skull, bounded on all sides by bone tissue. In adults it is quite voluminous, sometimes reaching 10 cm3. Its shape and location in the bones determine the unique pronunciation inherent in humans. The cavity, resonating, forms the timbre of sound.
The paranasal sinuses are lined from the inside with a thin mucous membrane and are connected to the nasal cavity by thin tubules for drainage of mucus and ventilation. If the holes become clogged, inflammation develops - sinusitis.
There are a number of known features that explain the appearance of a hole in the bottom of the maxillary sinuses:
- The size and thickness of the walls separating the maxillary sinuses from the oral cavity are individual for each person. With thinned bone (up to 1 mm thick), the sinus is easily perforated when the dentist works. This is also facilitated by the proximity of the roots of the front teeth.
- It happens that the roots of distant teeth penetrate into the sinus area and are separated from it only by a thin film of mucous tissue. As long as the tooth is healthy, everything is fine. If the doctor begins to manipulate the canals of such teeth, the mucous membrane breaks through and penetration occurs.
- Even healthy bone can atrophy and become thin and weak with persistent periodontal and periodontal diseases. Or the trabeculae of the upper jaw - the plates that form its skeleton - are insignificant from birth. It is easy to perforate such an obstacle with sharp instruments.
Therefore, it cannot be unequivocally stated that the doctor is always to blame for the development of complications.