Matteo Trimarchi Department of ENT and Head and Neck Surgery, San Raffaele Hospital, Milan, Italy
A. Galli Department of ENT and Head and Neck Surgery, San Raffaele Hospital, Milan, Italy
Paolo Cappare Department of Dentistry, IRCCS San Raffaele Hospital, Milan, Italy
Suzan Dababou Department of Dentistry, IRCCS San Raffaele Hospital, Milan, Italy
Raffaele Vinci Department of Dentistry, IRCCS San Raffaele Hospital, Milan, Italy
M. Bussi Department of ENT and Head and Neck Surgery, San Raffaele Hospital, Milan, Italy
Enrico Gherlone Department of Dentistry, IRCCS San Raffaele Hospital, Milan, Italy
Odontogenic infections (OIs) are pathologies originating from the stomatognathic system as a result of complications of dental pathologies or dental procedures. If they are not promptly diagnosed and treated, they can quickly spread throughout the head and neck and, depending on the etiology and the area where they begin, lead to severe, life-threatening complications [1-3]. For the development of OI, not only delayed diagnosis and inadequate treatment are important, but also common comorbidities of patients: diabetes, autoimmune or lymphoproliferative disorders, renal failure, osteoporosis, malnutrition, smoking, alcohol abuse and chronic steroid use - factors that can increase the incidence of OI [12].
OI can develop in both the upper and lower parts of the head and neck. The upper includes the spaces near the upper dental arch, namely the paranasal sinuses, with the maxillary sinuses being involved in most cases [4]. Odontogenic sinusitis (OS) accounts for about 10–30% of cases of chronic antral inflammation [2] and 8% of cases leading to endoscopic nasal surgery [5]. The lower section is characterized by the proximity of the lower dental arch to the fascial cervical spaces: superficial, submental, submandibular, sublingual, parapharyngeal, masticatory, carotid, retropharyngeal, prevertebral. And also to the dangerous space, which extends from the base of the skull to the posterior mediastinum [3, 6, 7]. Odontogenic etiology underlies 57% of cases of cervical-fascial infections [8].
Diagnosis of OI can be challenging: signs and symptoms are often nonspecific or misleading (especially for OI), and the association with overt dental pathology is often not seen or underestimated. Dental symptoms (local pain or hypersensitivity), in fact, do not reliably correlate with odontogenic etiology [2, 9]. This can lead to rapid and effective treatment, symptoms and severe complications [10]. The clinical picture is different between upper and lower OI. Pain/pressure, swelling of the posterior nasal wall, copious mucous discharge from the nose, nasal congestion, decreased/absent sense of smell and an unpleasant taste in the mouth are characteristic of the upper nasal region. While sore throat, pain when swallowing, shortness of breath, enlarged cervical lymph nodes and more serious involvement of other organs and systems characterize the lower one. Fever is often present [2 – 4, 7].
Accurate and clear diagnosis allows not only to identify the complication, but also the specific cause of the infection, which allows for correct treatment and reduces the risk of relapse [10].
In the present study, we analyzed the various pathogenesis that can lead to OI and highlight the importance of collaboration between dentists and otolaryngologists for the effective management of potentially dangerous complications.
Types of infections
Dentists divide diseases based on their development:
- truly odontogenic. They are caused by a problem tooth. If caries, pulpitis, periodontitis, inflammation are not cured in time, the infection begins to spread further;
- non-odontogenic. The reason is damage to the oral mucosa;
- periodontal. Advanced problems with the gums, periosteum or soft tissues of the neck are to blame for the occurrence of such infections.
Whole groups of microorganisms can be causative agents of infection: viridans streptococci, spirochetes, non-spore-forming anaerobes.
Causes of inflammation
Most inflammatory diseases of the maxillofacial area are associated with dental pathology. These include periostitis, osteomyelitis , lymphadenitis and others. As a rule, they arise as a result of various dental diseases or tissues surrounding the teeth. In addition, the causative agents of inflammatory infections can be staphylococci, streptococci, candida fungus and other microorganisms, including those that are present in the oral cavity of every person. Often, infection occurs due to defects in the surfaces of teeth: carious lesions. This becomes an entry point for infection. Complications are associated with the fact that tooth tissue is not able to recover naturally. Therefore, the longer you wait to go to the dentist, the higher the risk of developing inflammation.
Causes of development of odontogenic infections
More often, diseases spread and develop due to patients’ inattention to their health. The reasons are:
- infrequent visits to the dentist. Even if nothing worries you, you need to undergo medical examinations every six months. Professional oral hygiene in a dental clinic removes plaque, tartar, restores the natural shade of enamel and prevents the occurrence of caries and gum problems;
- poor hygiene and bad habits. When a patient does not spend enough time brushing his teeth, does not use dental floss, and self-medicates instead of visiting a specialist, the condition of the oral cavity worsens. Smoking and drinking alcohol have a bad effect on the gums: the tissue becomes thinner, becomes inflamed and begins to bleed;
- unsuccessful dental operations. Serious problems can result from an incorrectly placed filling, traumatic tooth extraction, incompletely cured caries or other disease.
Your dentist will help determine the cause. The specialist will also give recommendations on how to avoid problems in the future.
results
In 29 cases (90.7%) the result of OA was sinusitis, in 2 - palatal abscess (6.2%) and canine fossa abscess (3.1%). The cervical-fascial spaces were involved as follows: submental space in 2 cases (16.7%), submandibular in 7 cases (58.3%), sternocleidomastoid region in 2 cases (16.7%), and peripharyngeal with descending spread into the mediastinum in one (8.3%).
Causes of OI included tooth extraction (7 cases - 15.9% overall), installation of implants (13 cases - 29.6%), caries (12 cases - 27.3%), eruption anomalies (8 cases - 18.2% ), endodontic manipulations (2 cases - 4.5%), as well as sinus lifting (2 cases -4.5%). They are also divided into complications of pre-implantology (2 cases - 4.5%) or implantology treatment (13 cases - 29.6%), consequences of “classical” dental procedures (i.e. tooth extraction, endodontics), caries or eruption anomalies ( 29 cases - 65.9%), according to the proposal of Felisati's classification [11].
Microbiological cultures of surgical specimens were negative in 5 cases (11.4%) or showed nonspecific growth of mixed oropharyngeal flora (OP) in 12 cases (27.2%). Thus, antibiotic therapy was used in most patients. Three (6.8%) purely mycotic infections (Aspergillus spp) were observed as mycetomas of the maxillary sinus.
Cervical surgical drainage with removal of necrotic tissue in combination with dental procedures aimed at eliminating concomitant dental pathologies was used in all cases of detection of oropharyngeal flora (12 cases). Recurrent infection developed in one case after surgery (ie, parapharyngeal abscess as a consequence of long-standing, untreated caries), with retropharyngeal and subsequent descending mediastinal spread. The patient required additional thoracotomy and an extended stay in the intensive care unit.
Conversely, in case of upper segment OI (32 patients), access was created through a functional endoscopic transnasal approach in 11 cases (34.4%) or using a combination of FEC and the Caldwell-Luc approach (18 cases - 56.2%). Three upper ROIs (two hard palate abscesses and one canine fossa abscess - 9.4%) were eliminated by transoral surgical drainage without FEC.
Signs of infection and patients at risk
Main symptoms:
- I constantly have a high temperature and a headache. These are signs of intoxication of the body;
- notice a purulent focus. Redness appears around, the affected area swells and hurts.
Problems also begin in the neck area: the throat hurts, the tongue swells, it becomes difficult to breathe and speech is distorted. Often with such complaints they go to a general surgeon. The doctor helps eliminate the consequences of the infection, but the outbreak still remains, and the disease continues to spread through the vessels and affect the tissues.
People with weak immunity are considered the most vulnerable to odontogenic infections: patients with oncology, hepatitis, HIV, diabetes. By age group, children and patients over 60 years of age are at greatest risk. Chemotherapy and drugs that suppress the immune system also weaken the body.
Treatment of inflammatory diseases in Kaluga
If any symptoms of the above diseases occur, it is important to consult a doctor immediately. Even a day of delay can result in serious complications. An oral and maxillofacial surgeon working in our clinic will conduct a thorough examination and prescribe competent treatment. Make an appointment by phone or through the feedback form on the website.
We are always happy to help you and invite you to medical assistance! Be alert! You can make an appointment by phone; 8 (4842) 27-72-50.
How are odontogenic infections treated?
The dentist begins with sanitation of the oral cavity, then carefully opens the abscess. Treatment of dental infections is carried out using different methods depending on the degree of complexity and location of the outbreak. One of the principles is to provide air flow, which will kill pathogens.
If the abscess is too deep in the tissues, the process is monitored using ultrasound. Patients are required to be given antibiotics. Then they are combined with antimicrobial drugs. General strengthening therapy is also used.
If the infection is not treated in time, you may encounter complications:
- purulent inflammations,
- blockage of veins,
- sinusitis,
- damage to the lymph nodes,
- sepsis.
To avoid odontogenic infections, visit your dentist regularly, do not delay treatment, and carefully monitor your oral health.
Discussion
The oral cavity is an anatomical region with a high presence of bacteria. For example, the number of microorganisms in a periodontal pocket can reach 1.8 x 1011/g of material [12]. Therefore, all oral procedures should be performed to minimize the risk of secondary infections and possible systemic bacterial spread.
OIs are often encountered in everyday dental practice, especially in adults: odontogenic pathogenesis is detected in 10-30% of cases of sinusitis [2] and in almost 50% of cases of cervical-fascial infections [6]. However, their prevalence remains largely underestimated due to their nonspecific clinical presentation compared to their nonodontogenic counterparts and unpredictable course [2, 6].
As stated previously, OIs are potentially invasive complications due to the proximity of the oral region to other anatomical spaces of the head and neck, namely the paranasal sinuses (superior OI) and the deep cervicofascial spaces (inferior OI) [2-7]. In our sample, the main causes of OI were implantation (13/44, 29.6%) and caries (12/44, 27.3%), followed by eruption anomalies (8/44, 18.2%), tooth extraction (7/ 44, 15.9%), endodontic procedures (2/44, 4.5%) and sinus lift (2/44, 4.5%). However, stratifying the pathogenesis by the areas involved, implantation becomes predominant when determining OH (11/32, 34.4%), and caries - when involving the cervical-fascial spaces (7/12, 58.3%). This conclusion is consistent with literature data [6, 13].
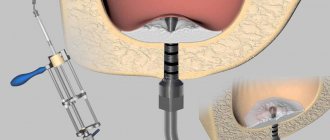
The use of implants for rehabilitation has increased significantly in recent years. This type of rehabilitation is very useful and successful, also in immunocompromised patients [14], but implantation is not always easy or safe to perform, especially by inexperienced surgeons [4]. Superior displacement of the implant (Fig. 1 a, b) may, in fact, perforate Schneiderian membrane, leading to a foreign body reaction and altering sinonasal mucociliary clearance. Thus, stasis of inflammatory components within the sinus causes OH [14, 15]. A similar condition easily occurs with an atrophic alveolar process [13, 16] or with concomitant sinonasal pathology (i.e., decreased patency of the nasal passages due to deformation of the septum, turbinates, cribriform plate) (14). Moreover, even a well-placed implant in a patient with major risk factors (eg, pre-existing sinonasal pathology, diabetes, malnutrition, smoking, steroid therapy, osteoporosis) can lead to OI [1], as can failed pre-implant procedures [4, 14]. , 17]. Indeed, sinus lifting with bone graft can lead to severe OI [4, 14, 17].
Rice. 1 a. The upper implant is displaced into the cavity of the maxillary sinus.
Rice. 1 b. The upper implant is displaced into the cavity of the maxillary sinus.
While many dentists are aware of the possible complications after implant placement, caries and eruption abnormalities are largely underestimated. However, these are common causes of OI, as confirmed by the study results. When caries remains untreated for a long time, the bacterial load is high and underlying conditions exist (eg, caries, periodontal disease, diabetes, immunosuppression), spread of infection from the dental hard tissues into the pulp and periodontal tissues may occur, facilitating subsequent diffusion through the alveolar bone into the cervical fascial spaces [6, 18]. The same applies to eruption anomalies [19] (Fig. 1c, d), which can contribute to OH, cyst formation and granulomatous inflammatory response [20] or traumatic injuries associated with the extraction of affected teeth [16, 21]. The deep spaces of the neck, in particular, are potential areas of low resistance that fill with inflammatory exudate and pus in the event of infection, causing airway narrowing, descending mediastinal or systemic spread, erosion of large blood vessels and life-threatening thrombosis/hemorrhage, with significant mortality up to 40% of cases [6].
Rice. 1st century Molars in the maxillary sinus cavity (white arrows), a clear example of eruption anomalies in the maxilla.
Rice. 1 g. Molars in the cavity of the maxillary sinus (white arrows), a clear example of eruption anomalies in the upper jaw.
Tooth extraction can also cause OI [11, 12, 22]. If not performed correctly, this procedure can lead to alveolitis, displacement of the tooth root into the maxillary sinus (Fig. 2) [11, 12, 22]. Risk factors include the presence of radiating roots, dental caries, and large fillings, as these conditions may contribute to tooth fracture [22].
Rice. 2 a. An endoscopic probe approaching an oroantral fistula resulting from improper tooth extraction.
Rice. 2 b. Purulent discharge from the fistula as a result of the insertion of a probe.
Another cause of OI (especially OH) is endodontics, the materials or instruments of which can exit the apex of the root canal, reaching the maxillary sinus. This often results in fungal colonization of the sinus, with fungal granuloma being the most common clinical manifestation [23–25]. In our series, we observed 3 mycetomas of the maxillary sinus (Fig. 3) as a result of unsuccessful endodontic procedures (2/3) or implant placement (1/3).
Rice. 3 a. Mycetoma of the maxillary sinus resulting from unsuccessful endodontics.
Rice. 3 b. Removal of mycetoma followed by drainage of the sinus.
Rice. 3rd century Typical CT scan for complete inflammatory obliteration of the sinus.
Rice. 3 g. Fungal colonization sample.
Rice. 4 a. Periapical periodontitis on the lower jaw on the right with an accompanying abscess spreading from the submandibular space to the buccal space.
Rice. 4 b. Periapical periodontitis on the lower jaw on the right with an accompanying abscess spreading from the submandibular space to the buccal space.
The etiologies of our OIs are consistent with other studies known in the literature [26, 27]: alpha-hemolytic streptococcus was most often found in purulent contents (9/44, 20.6%), followed by beta-hemolytic streptococcus (S. pyogenes and S. agalactiae; 6/44, 13.6%), gram-negative species (K. pneumoniae, E. corrodens and Enterobacter spp; 6/44, 13.6%), Staphylococcus aureus (4/44, 9.1%) and obligate anaerobes (2/44, 4.5% ). Pathological samples did not yield growth in 5 cases (11.4%), nonspecific mixed oropharyngeal flora was isolated in 12 cases (27.2%); this circumstance is not unusual [26, 27], since OIs are often polymicrobial [2]. This makes the choice of antibiotic particularly difficult and necessitates the need for combination, intravenous therapy with broad-spectrum antibiotics.
As for OI of the cervicopharyngeal spaces, several “red flags” almost always need to be noted in treatment: rapid progressive edema, worsening of the trismus, dyspnea/tachypnea, dysphonia, dysphagia, pyrexia or neck stiffness - all these are clear signs of a complex course and should be promptly addressed eliminated to avoid deterioration and risk of death [6, 7]. In our sample, there was a case of recurrent infection after successful drainage of a parapharyngeal abscess with retropharyngeal and subsequent descending mediastinal spread. A multimodal approach and prolonged intensive care unit stay with aggressive intravenous therapy were required. Timely detection of worsening clinical course was necessary to save the patient. A high index of suspicion should always be maintained when treating OI of the cervicopharyngeal spaces, even after apparently successful drainage: vital signs, temperature, complete blood count, neck palpation and laryngoscopy should be repeated regularly in the postoperative period [6, 7].
Odontogenic sinusitis often requires the creation of several surgical approaches (transnasal endoscopic approach in combination with transoral) [11]. In our sample, this circumstance occurred in half of the cases (16/32, 50.0%). The Caldwell-Luc approach has now been practically abandoned due to greater trauma, and is performed in the presence of large foreign bodies in the cavity of the maxillary sinus [28, 29]. In fact, we used this procedure in few cases [2/32, 6.2%].
Complications
With odontogenic sinusitis, a chronic inflammatory process occurs. Dental microflora appears in the sinus, not typical for the upper respiratory tract, which can destroy bone tissue. Due to the fact that the paranasal sinuses have contact with the orbit and brain, odontogenic sinusitis can lead to severe complications:
- intraorbital (orbital phlegmon, ophthalmitis, optic nerve neuritis);
- intracranial (meningitis, encephalitis, brain abscess).
Therefore, at the slightest suspicion of this disease, you should consult a doctor.
Recovery after surgery
No hospitalization
A hospital stay for 2-3 days after surgery (as happens in city hospitals) is not required.
Gentle surgical protocols, the use of modern functional equipment and a microscope allow treatment to be carried out as delicately as possible .
All operations are performed in a controlled, drug-induced sleep - this is not general anesthesia ! Recovery from the state is easy, without dizziness, memory loss or clouding of consciousness. The drugs are absolutely safe for the body and are eliminated naturally 40 minutes after stopping the supply.
For patients with vascular and cardiac problems, a day hospital , where you can calmly recover and recover under the supervision of our anesthesiologist-resuscitator.
Accelerated rehabilitation
Recovery after the intervention occurs within a week. For those who want to speed up the process, our Center provides a set of procedures to reduce pain, resolve hematomas and swelling - carried out on the day of surgery.
Home care
Medications are prescribed - antibiotics, painkillers and decongestants. To prevent the patient from running to pharmacies in a postoperative state and to avoid purchasing counterfeit products “on the side,” the entire package of drugs is collected and given out free of charge .
The package contains all the necessary medications for taking and caring for the surgical area.
Please follow the recommendations and do not skip taking medications to avoid complications. The instructions are in the medicine package.
If you suspect a worsening condition, contact the clinic immediately. The telephone number for the 24-hour patient support service is listed in the memo.
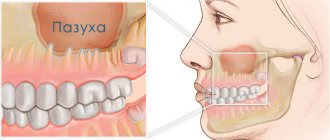
What are the maxillary sinuses
The maxillary sinuses (also called the maxillary sinuses) are special cavities on both sides of the nose that are filled with air. Each cavity is connected to the nasal passage by small openings called anastomoses. The cavities are covered with mucous membrane. The function of mucus is to trap bacteria and harmful particles in it, and then remove them from the body through those same anastomoses. When edema occurs, the excretory opening becomes very narrow, as a result of which mucus, along with harmful particles and bacteria, cannot come out and stagnates. At this time, the patient begins to experience bursting pain in the cheek area - this is how inflammation of the maxillary sinus begins. Treatment of the maxillary sinus should not be neglected, since inaction can provoke serious consequences, including sepsis and meningitis.
Classic sinusitis can be bilateral, when both sinuses are affected. In the odontogenic form, the inflammatory process starts in the sinus on which side the diseased tooth is located.
Symptoms of odontogenic sinusitis
Most often patients complain of:
- moderate pain in the cheek or infraorbital region (sometimes the entire half of the face hurts);
- nasal congestion on one side only, feeling of heaviness;
- discharge of pus from the corresponding half of the nose;
- pain when biting on an incorrectly treated tooth;
- dysfunction of the sense of smell;
- feeling unwell – headache, fever, sleep disturbance, chills;
- With an exacerbation of the disease, enlargement of the lymph nodes on the corresponding side is possible.
Patient management tactics
The “gold standard” for diagnosing odontogenic sinusitis is computed tomography of the paranasal sinuses, which allows not only to establish the fact of inflammation of the mucous membrane of the maxillary sinus, but also to exclude the presence of a foreign body (for example, filling material) in the sinus, and also to determine the role of dental pathology at the moment. Treatment of such patients requires teamwork between a dentist and an otolaryngologist, each of whom undertakes therapy within the scope of their professional competence. With properly selected therapy, it is often possible to solve the problem conservatively, but sometimes surgical treatment is required, which is also carried out by a dentist + ENT team.
Despite some difficulty in diagnosis, treatment of odontogenic sinusitis, as a rule, leads to complete recovery, and the patient does not require long-term medical supervision. On the other hand, periodic examination by a dentist is a necessary condition for the prevention of this pathology, even in the absence of a history of this disease.
Be healthy!