Almost every person on earth has experienced toothache at least once. It can be very difficult to tolerate, and sometimes simply unbearable. To avoid complications, one of which may be periodontitis, you should immediately consult a doctor.
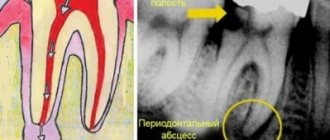
Periodontitis is an inflammatory process of the apex of the tooth root, as well as in the tissues adjacent to it. This is a rather dangerous disease that can lead to even more serious problems, so you should not delay treatment. Periodontitis can occur as a result of advanced pulpitis or poor-quality canal filling.
Also, the causes of this disease can be an infection, injury, or the consequences of medication. According to statistics, this disease accounts for 45-50% of all dental diseases. People with weakened immune systems are most susceptible to rapid development of the disease.
Symptoms of periodontitis
It is impossible not to notice the symptoms of periodontitis. These include:
- The occurrence of severe pain that is constant;
- The appearance of painful sensations when chewing or touching;
- A clear feeling of which tooth hurts, with a feeling of bursting from the inside;
- Discharge of a small amount of fluid from under the tooth, accumulation of pus in the gums;
- The pain may be throbbing and radiate to the temporal or ear region;
- Bad breath;
- Visible swelling and redness of the gums.
When should you see a doctor?
Have you recently had a root canal treatment? Does your tooth hurt a lot after periodontitis treatment? Do the unpleasant sensations persist? Make an appointment with your dentist. The specialist will conduct a diagnosis and determine the exact cause of the pain syndrome. If errors were made during treatment, the canals will have to be re-processed and filled.
You should also consult your doctor:
- if the tooth loosens easily,
- When closing the jaws and chewing, there is a sharp pain,
- the gums are very swollen, the lip or cheek is swollen,
- body temperature rises to 38-39 degrees,
- health deteriorates significantly.
You should not endure toothache and drown it out with pills. It may indicate pathological processes occurring inside the tooth. You need to see a doctor and get medical help as soon as possible.
Types of periodontitis
Depending on the nature of the processes occurring in the area of the tooth root, periodontitis has three forms.
- Chronic fibrous. A type of chronic periodontitis. This disease most often affects older people. The disease is practically asymptomatic, but during an exacerbation, pain may occur when chewing food. This form of periodontitis is manifested by fibrous changes in the periodontal tissue, that is, the tissue around the tooth becomes pale pink, and the tooth itself may become gray.
- Chronic granulating. It is also a chronic form of periodontitis. It is often the cause of complicated caries, and is characterized by inflammation in periodontal tissues. In this case, granulation tissue appears, which grows and can have devastating consequences for the bone.
- Granulomatous. Chronic stage of periodontitis with an inflammatory nature. Granulomas appear in the tissues at the apex of the tooth root, that is, formations that separate the infectious focus from part of the healthy tooth. Gradually, the tissue surrounding the tooth is destroyed.
In addition, according to the speed of the disease, periodontitis can be of the following types.
- Spicy. The disease acquires this form at the final stage. This form is characterized by rapid development, accompanied by acute pain (especially when eating hot food), redness and swelling of the gums, and the appearance of a fistula.
- Chronic. This form is characterized by sluggish processes due to unresolved inflammation. Pathogenic microorganisms constantly penetrate inside the tooth and contribute to its death, as well as damage to the tissues surrounding the tooth and bone destruction.
- Chronic in the acute stage. When the disease is in the acute stage, a person may experience a rise in temperature, a headache, a feeling of weakness, swelling of the gums and face, enlarged lymph nodes, and mobility of a damaged tooth.
Specialists who took part in the treatment:
- Dentist-endodontist – diagnosis of periodontitis, treatment of tooth canals under a microscope, tooth restoration with a ceramic inlay.
- ENT A.V. Arkhandeev – diagnosis and treatment of sinusitis.
- Dental assistant A. Antoshkina.
- ENT assistant E. Shilova.
See other examples of the work of specialists from the Dial-Dent clinic here.
Make an appointment for a consultation by phone +7-499-110-18-04 or through the form on the website. You can ask questions about dental treatment to the chief doctor of the clinic, Sergei Vladimirovich Tsukor, at
Treatment of acute periodontitis
Any form of the disease requires immediate treatment. Surgical treatment of acute periodontitis involves opening the tooth for free access to the canals and mechanical cleaning using local anesthesia. It is also necessary to treat the canals with an antiseptic or administer antibiotics if necessary. Several treatment sessions may be required, during which the tooth is either left open or covered with a temporary filling. After the inflammation and pain are eliminated, a permanent filling is installed, after which an x-ray must be taken.
In some cases, periodontitis is treated surgically. If the nerve becomes inflamed, it must be removed. After completing treatment, it is useful to rinse your teeth with a soda solution for some time. Unpleasant sensations may occur for several weeks after treatment. But soon they will pass. If no repeated problems arise within six months, we can assume that the disease has been eliminated. Thanks to modern medicine, relapses of the disease occur in only 15% of cases.
Dental periodontitis: what it is, how to treat it
| Treatment of periodontitis always begins with a doctor analyzing the patient’s complaints and studying the image. Only after this will it be possible to understand whether a tooth will need to be removed due to periodontitis, or whether it can be saved! |
Treatment of periodontitis: stages
- If the disease has reached an acute stage, then the doctor’s first priority is to create an opportunity for the pus to flow out, since otherwise it will not be possible to get rid of the acute pain.
- The crown (if any) is removed, the root canals are unfilled (this must be done on the patient’s first visit).
- If the gums are swollen, the abscess will need to be opened.
Open root canals will allow the pus to drain freely, which will significantly relieve the pain. In addition to this, the dentist will prescribe antibiotics and rinses. A repeat visit is scheduled no earlier than two to three days later. If the pus no longer drains by this point, an antiseptic drug is placed in the canals.
Further methods of treating periodontitis will largely be determined by the size of the inflammatory focus.
Treatment of acute periodontitis of the tooth
The acute stage of the disease is accompanied by severe pain, forcing the patient to consult a doctor as soon as possible.
During the visit, the doctor removes the pulp (the root canals are not closed, since a path is needed for the pus to exit). A crown or filling may need to be removed. If the gums are swollen, the dentist may decide to make an incision to facilitate the release of purulent masses.
In most cases, these measures are enough to make the pain go away. In addition to surgical measures, the patient is prescribed drug therapy in the form of taking oral antibiotics and rinsing with them.
After 4 days, a follow-up visit is scheduled, during which the doctor checks whether all the pus has come out. To achieve final cleaning, an antiseptic is placed into the tooth.
Then, with the help of medications, the inflammatory process is relieved, and the canals are sealed. In some cases, bone tissue restoration and long-term anti-inflammatory therapy may be required. Sometimes a doctor may find it advisable to get rid of a cyst using a laser.
Treatment of chronic periodontitis
Treatment of the fibrotic form involves several visits to the doctor over the course of a week. Since the upper part of the root is not changed, the technique allows you to fill the canals at the next visit to a specialist.
But the treatment process for granulating and granulomatous periodontitis can take a couple of months, especially if there is a complication.
The following procedures are carried out first:
- a picture is taken;
- under anesthesia, carious areas are drilled and access to the canals is provided;
- if the tooth has not been treated, the pulp is removed, if it has been filled, then the canals are unsealed;
- the channels are expanded and treated with an antiseptic solution;
- until the patient’s next visit to the doctor, an antiseptic is placed in the canals (usually Cresophenon is used);
- a temporary filling is placed;
- Anti-inflammatory drugs may be prescribed (but this is not always done).
The next visit is scheduled in three days:
- the previously placed temporary filling and the medicine placed in the canals are removed;
- the channels are thoroughly washed with antiseptics;
- The canals are filled and then a temporary filling is placed again.
On last visit:
- a picture is taken that makes it possible to understand how successful the tooth restoration after periodontitis was;
- The filling material is removed from the canals and treated with an antiseptic;
- the channels are sealed;
- Another picture is taken to determine whether the canals have been sealed to their entire length, otherwise the disease may begin again after some time.
If the size of the cyst exceeds 1.5 cm (cases have been recorded when the formation can grow up to 5 cm), then after filling, root resection and subsequent restoration of the tooth are performed.
Treatment of chronic periodontitis
Before starting treatment for chronic periodontitis, it is necessary to conduct a thorough examination of the patient. To do this, probe and x-ray of the affected area of the jaw are performed. Based on the results, an effective treatment method is prescribed.
Periodontitis is treated in two ways.
- Treatment of the disease with a therapeutic method involves the use of antibacterial medications that have a wide spectrum of action, localize inflammation and relieve symptoms. Periodontal canals inside the tooth are treated with antiseptics, and general strengthening drugs are also used to accelerate tissue regeneration. It is also possible to use laser processing. Treatment lasts up to six months. The dynamics are monitored using x-rays.
- The surgical method is used if therapeutic treatment does not produce the desired results. It consists of removing the affected tissue, resection of the apex of the tooth, or its complete removal. If there is a large amount of pus, installation of elastic drainage is required. After the procedure, the patient must take medications prescribed by the doctor to avoid infection and to accelerate tissue regeneration.
Pain after REMOVAL of a “NERVE” from a tooth (after treatment for PULPTIS).
Quite often, so-called “post-filling” pain occurs after tooth depulpation. Mild pain when pressing on a tooth is considered normal.
and tapping on it, lasting no longer than 4–8 weeks. This is due to the fact that during the treatment process the doctor performs mechanical treatment of the root canals with metal instruments and rinses the canals with powerful antiseptics. All this can irritate the tissue surrounding the root. The reaction to such influences is different for all patients.
If the pain when biting on a tooth is sharp, severe, there is a feeling of an “overgrown” tooth, swelling of the gums or cheeks around the tooth appears, general health worsens or body temperature rises - this is a reason to immediately consult a doctor. Complications of endodontic treatment may have arisen that need to be addressed.
Mistakes in the treatment of periodontitis
Medical errors acceptable in the treatment of periodontitis, or errors arising for other reasons, can cause complications such as the appearance of a fistula, cyst and osteomyelitis. These complications are called local. But there are also general complications. These include intoxication of the body and infection (sepsis) of the blood. Therefore, to treat a disease such as periodontitis, you should contact only qualified specialists. All complications that arise during the treatment of periodontitis require immediate medical intervention. Let's take a closer look at local complications.
- Fistula. A fistula occurs as a result of poor-quality tooth filling, which causes bacteria to multiply inside it. An inflammatory process appears and a fistula is formed, through which pus is released. Treatment is carried out by taking antibiotics and antihistamines, as well as rinsing with saline solution. If treatment is carried out correctly, the fistula will close on its own.
- Cyst. The formation that occurs in the upper part of the tooth is called a cyst. It develops slowly and does not cause concern. As the size of the cyst increases, complications begin. The cyst is diagnosed using an x-ray and removed surgically using local anesthesia.
- Osteomyelitis. An infectious disease that can lead to the breakdown of the jaw bones. Diagnosis requires a complete examination, including a blood test, x-rays and other tests. For treatment, it is necessary to remove the diseased tooth and then take antibiotics.
It is known that the best prevention of diseases is their prevention. You shouldn’t put off going to the dentist for a long time, even if you have minor caries. Take care of your teeth, and then you will avoid serious dental diseases, have healthy teeth and a beautiful smile.
Possible causes of pain
After treatment of periodontitis, discomfort may persist for 7-14 days. This is due to injury to the tooth tissue. If you follow the recommendations of your doctor, regeneration will accelerate and discomfort will disappear.
If the pain persists for longer, you should consult a specialist. The main reasons for this problem include:
- poor-quality filling – lack or excess of filling material;
- the presence of foreign bodies in the root canals – most often these are elements of dental instruments;
- the emergence of a new focus of inflammation - due to the spread of pathogenic bacteria, tooth tissue can become inflamed again.
These are the most common causes of tooth pain after treatment. A doctor will help determine the provoking factor.