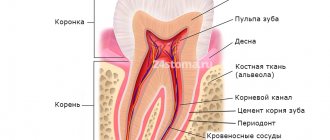
Anatomically, a tooth consists of three parts:
- crown
- neck
- root
There is a cavity inside the crown and root. The pulp is localized in these cavities. The part of the pulp that is in the crown is called coronal, and in the root is called root.
The pulp itself consists of nerve endings, blood vessels and lymphatic vessels.
The pulp is the nerve of the tooth, together with blood and lymphatic vessels, providing the tooth with nutrients.
Inflammation of the pulp is called pulpitis.
Causes of pulpitis
The causes of pulpitis are varied. Bacterial infection comes first. Bacteria enter the pulp through carious cavities, through dentinal tubules after preparation, when taking an impression under pressure, as well as microbes entering through the apical foramen (infection of the pulp through the apical foramen), for example, in case of sepsis, osteomyelitis, after curettage of deep periodontal pockets, etc. d.
Irritation and trauma during the treatment of caries and during the preparation of teeth under fixed dentures, the toxic effect of filling material, dental trauma due to a fracture or crack of a tooth.
Types (classification) of pulpitis
In 1989, the MMSI proposed the following classification of pulpitis:
1. Acute pulpitis:
- a) acute focal pulpitis;
- b) acute diffuse pulpitis.
2. Chronic pulpitis:
- a) chronic fibrous pulpitis;
- b) chronic hypertrophic (proliferative) pulpitis;
- c) chronic gangrenous pulpitis.
3. Exacerbation of chronic pulpitis.
In Russia, the transition to ICD-10 was carried out in all health authorities and institutions in 1999.
The diagnosis is indicated according to ICD-10. In brackets you can indicate the corresponding form of pulpitis according to MMSI.
Diagnosis of acute pulpitis
Various methods are used to diagnose acute pulpitis.
Basic research methods.
During the survey, it is important to establish the so-called “pulpitis” nature of the pain.
During the examination, a deep carious cavity is discovered (with an infectious cause of pulpitis).
Probing its bottom is sharply painful at one point or over the entire surface. Possible perforation into the tooth cavity.
The reaction to percussion is still painless in case of partial pulpitis, slightly painful in the case of general pulpitis, painful in case of purulent pulpitis.
Palpation of the transitional fold is painless.
Additional research methods include studying the reaction to temperature stimuli, electrical excitability, and radiography. Temperature stimuli provoke an intense, prolonged pain attack.
Electroodontodiagnosis indicators: 20-25 µA for acute focal pulpitis (the value may be normal in the area of another tubercle, on the side of the not yet inflamed pulp). Acute diffuse pulpitis corresponds to values of up to 30-40 μA or more.
Radiography is effective for determining the location of a hard-to-reach carious cavity (contact surface) in relation to the tooth cavity. It also helps to identify periodontal pockets and inflammation in the periapical tissues. This is useful in the differential diagnosis of acute forms of pulpitis.
Classification of pulpitis according to ICD-10
- K04 – diseases of the pulp and periapical tissues
- K04.0 – pulpitis
- K04.00 – initial (pulp hyperemia), and (according to MMSI deep caries)
- K04.01 – acute (according to MMSI acute focal pulpitis)
- K04.02 – purulent (pulp abscess), (according to MMSI acute diffuse)
- K04.03 – chronic (according to MMSI chronic fibrous pulpitis)
- K04.04 – chronic ulcerative pulpitis (according to MMSI chronic gangrenous pulpitis)
- K04.05 – pulp polyp (according to MMSI – chronic hypertrophic (hyperplastic) pulpitis)
- K04.08 – other specified pulpitis
- K04.09 – pulpitis, unspecified
- K04.1 – pulp necrosis (pulp gangrene)
- K04.2 – pulp degeneration (denticles, pulp petrification)
- K04.3 – improper formation of hard tissues in the pulp (secondary or irregular dentin)
Acute pulpitis in children
Symptoms of acute pulpitis in children are somewhat different from those in adults. This is due to the structural features of hard tissues and pulp of temporary or permanent teeth with unformed roots.
Firstly, acute pulpitis in children is rare, mainly in healthy children with low caries activity. Partial pulpitis is an even rarer phenomenon, because the barrier between the root and coronal pulp is immature. Serous pulpitis very quickly turns purulent.
Secondly, the tooth cavity is always closed, the carious cavity is filled with light infected dentin.
Thirdly, in children, acute pulpitis is often accompanied by a periodontal reaction, swelling of the soft tissues surrounding the tooth. Regional lymph nodes become inflamed. The general condition worsens: inflammation spreads to the bone tissue.
Finally, the most common outcome of acute pulpitis of primary teeth is pulp necrosis.
Clinical picture of initial K04.00
There is no history of spontaneous pain. When interviewed, it turns out that pain comes from various irritants, which quickly goes away after they are eliminated. A painful attack is provoked by cold and hot stimuli (temperature). Almost always the patient points to the causative tooth.
Pain from temperature stimuli quickly (within a few seconds) goes away. When talking with the patient, it turns out that the tooth has not hurt before.
- The tooth cavity is not opened.
- Percussion is painless.
- Probing is painful at one or more points.
- Electroodontometry - 10-12, and sometimes 20 microns (normally 2-6 microns).
- X-ray – no changes.
Differential diagnosis of acute pulpitis
Differential diagnosis of acute pulpitis is carried out with various diseases. Although the symptoms of acute pulpitis are pronounced and specific, there are similarities with other pathologies. However, in making the correct diagnosis, it is more important to pay attention to the following differences:
Pulp hyperemia
With pulp hyperemia (deep caries), there is no spontaneous night pain reaction. A short painful attack is provoked by external stimuli.
Gingivitis
The presence of inflamed, swollen gums, gingival papilla, and associated pain is a manifestation of papillitis or gingivitis.
Acute apical periodontitis
Acute apical periodontitis is also accompanied by pain, but of a different nature. It is constant, aching, and worsens when biting. Palpation of the transitional fold is also painful. There is no reaction to external stimuli. The result of electroodontodiagnostics is a response with a value of more than 100 microamps.
Trigeminal neuralgia
With trigeminal neuralgia, pain occurs when certain “trigger” areas of the face are touched.
Sinusitis
Sinusitis (sinusitis) is manifested by deterioration of health, fever, and headaches. Breathing is difficult, purulent exudate is released. When you tilt your head forward, heaviness and bloating appear. The localization of these symptoms is the area of the maxillary sinus. The x-ray shows characteristic changes in the sinuses.
Alveolitis
A strong pain reaction can also manifest itself with alveolitis. An examination helps to detect the socket of a recently removed tooth. The socket is covered with a gray coating, there is no blood clot. Characterized by an unpleasant odor. Palpation of the gums in its area is sharply painful.
Treatment of initial K04.00 (pulp hyperemia),
For initial pulpitis, conservative treatment is carried out.
Mostly preparations containing calcium hydroxide are applied to the bottom of the cavity, and then filled with permanent fillings, it is better to monitor after three months.
Clinical picture of acute K04.01 (according to MMSI acute focal) pulpitis
- Complaints: prolonged pain from all irritants, mainly at night. There are also spontaneous pains.
- The pain is clearly localized, the light intervals can last for several hours, and later these light intervals become shorter.
- When the chewing teeth (molars) are inflamed, pain during an attack can spread (radiate) to the ear, temple, and teeth of the opposite side (antagonist teeth).
- Inspection - deep carious cavity, a lot of softened dentin, which, when removed, can open the pulp chamber.
- Percussion is painless
- EDI – 25-40 or within normal limits
- Probing is painless
Treatment of acute K04.01 (according to MMSI acute focal) PULPTIS
The first thing you need to do is stop the inflammatory process, that is, stop the inflammation.
First, painkillers are prescribed to reduce or relieve pain.
First way.
In young people, at the beginning of the inflammatory process, it is possible to stop the inflammatory processes and preserve the pulp using conservative processes. To do this, the carious cavity is prepared with modern instruments that are available in our clinic, and then
is treated with medication and an anti-inflammatory, regenerating and odonotropic paste is applied, mainly based on calcium hydroxide paste for 4-6 days, and then if there are no complaints, the tooth is filled with permanent fillings.
Second way
When performing this method, first infiltration or conduction anesthesia is carried out, and then the softened tissues of enamel and dentin, as well as the inflammatory pulp at the level of the canal mouth are removed with a diamond bur, then the tooth cavity is cleaned, the bleeding stops and a paste based on calcium hydroxide is applied without any pressure. And ionomer cement is applied to it. The first control after three, and the next controls after 6 months and 1 year.
This method is called vital pulp amputation or pulpotomy .
Clinical picture of acute purulent K04.02 (pulp abscess) (according to MMSI acute diffuse) pulpitis.
- spontaneous pain;
- prolonged pain with short light intervals;
- radiating pain along the branches of the trigeminal nerve;
- intense, unbearable pain;
- increased pain from hot foods;
- short-term relief of pain from cold;
- EDI 30 – 50 mA;
- deep carious cavity with a large amount of softened dentin;
- the tooth cavity is not opened;
- probing is painful;
- percussion is painless;
- palpation of the transitional fold at the level of the inflammatory tooth is painless, but may be sensitive;
- with unformed root apices, percussion and palpation are painful;
- Severe swelling and disturbances in the general condition of the whole body may be observed.
- X-ray – no changes;
Clinic of acute pulpitis
The clinic of acute pulpitis is specific, the symptoms are vivid. This helps in making the correct diagnosis and selecting the right treatment method.
The main symptom is acute, unbearable, spontaneous, “evening” or “night” pain. The presence of external stimuli is not necessary for its occurrence. If irritants are present, the painful attack lasts for a long time even after their effect is eliminated. The pain alternates with “light”, pain-free periods.
Acute focal pulpitis
Acute focal pulpitis (partial) is the initial stage of acute inflammation of the pulp. Its focus is located closest to the deep carious cavity (pulp horn). Probing the bottom in this place is extremely painful. The tooth cavity, as a rule, is not opened. The peculiarity of this stage of pulp inflammation is short attacks of pain with long pain-free intervals (10-30 minutes and several hours). The pain does not radiate, and the patient correctly identifies the causative tooth. This stage lasts no more than 2 days.
Acute diffuse pulpitis
Further, inflammation takes over the entire pulp, and pulpitis becomes “acute diffuse (general).” Therefore, probing is painful along the entire bottom of the carious cavity. Now the duration of the painful period is increasing, and pain-free intervals are periods of time no more than 30-40 minutes. The pain may not go away, but only subside. The patient finds it difficult to identify the causative tooth; the pain radiates along the branches of the trigeminal nerve and even to the opposite side of the jaw. Possible deterioration in general health. Such a clinic of acute diffuse pulpitis can last up to two weeks.
Acute purulent pulpitis
An abscess can form in the tooth cavity as a result of inflammation. In this case, they speak of the occurrence of acute purulent pulpitis. With this disease, the nature of the pain changes slightly. It becomes pulsating, tearing, intensifying, and only subsides during pain-free intervals. There may be no pain-free periods at all: the pain lasts until the whole day or night. There are different reactions to stimuli. Cold soothes pain, heat provokes it. Clinically, the bottom of a deep carious cavity is covered with softened pigmented dentin. When probed, it easily perforates and purulent exudate is released. After this, the pain gradually subsides. Also characteristic is the appearance of a painful reaction of the tooth to percussion - the initial symptoms of apical periodontitis. Possible increase in body temperature.
The outcome of acute pulpitis is death (necrosis) of the pulp or chronicity of the inflammatory process (chronic pulpitis).