Vulvovaginitis
Vulvovaginitis is a disease of the female genital organs.
Inflammation may be of bacterial origin or be the result of mechanical irritation of the vulvar and vaginal mucosa. The natural structure of the female body allows us to protect the genitals from microorganisms from the external environment. The vaginal microflora of a healthy woman easily inhibits the growth of opportunistic bacteria that live on the mucous membranes. A decrease in immunity due to stress, intoxication or a viral disease can provoke a surge in the activity of pathogens, resulting in the development of acute vulvovaginitis.
Causes of the disease
Inflammation of the vulva and vagina appears due to the influence of such factors:
- violation of intimate hygiene rules, wearing underwear made of low-quality synthetics
- frequent change of sexual partners without the use of barrier contraception
- diseases of the metabolic system that can affect the vaginal microflora (diabetes mellitus, thyroid problems)
- hormonal imbalances characteristic of puberty and menopause
- taking antibacterial drugs (while taking antibiotics, a fungus like Candida is activated)
- chemotherapy and radiation therapy
- intoxication due to chronic infectious diseases
- mechanical injuries of the vulva and vagina, especially regular ones
The presence of more than two risk factors increases the likelihood of the occurrence of pathology several times.
Allergic vaginitis is also possible. Pathology is diagnosed in the presence of helminths.
Composition and release forms
The active ingredient of the drug has a long scientific name - dioxomethyltetrahydropyrimidine. It stimulates the activity of the immune system, has the ability to accelerate the division of healthy epithelial cells, prevents the accumulation of exudative masses, and reduces inflammatory tissue reactions in various pathologies and injuries.
Methyluracil is available in several forms:
- Ointment for external and local use: contains 10% active substance, petroleum jelly, lanolin and water. It is a yellow or yellowish-white oily viscous mass with a characteristic medicinal odor. Packaged in metal tubes or jars weighing 25–50 g.
- Suppositories: torpedo-shaped suppositories of light yellow color with a waxy texture, with a dosage of the active substance of 500 mg, containing solid paraffin, petroleum jelly and other auxiliary components. Packaged in contour plates with cells, the cardboard packaging of the drug contains 10 suppositories.
- Methyluracil tablets: with a dosage of 500 mg, flat-cylindrical, uncoated, white, bitter in taste. Packaged in 10 pieces in metallized blisters and cardboard packaging.
You can buy 10% Methyluracil ointment in pharmacies without a prescription, but to obtain the drug in tablets and suppositories you will need a doctor's prescription.
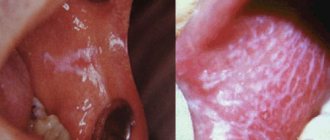
Vulvovaginitis: symptoms
Symptoms do not depend on the cause of the disease. Signs of an inflammatory process in the vulva and vaginal mucosa:
- itching
- burning
- painful sensations in the area of the external genitalia, aggravated by walking
- pain during intercourse
- scanty purulent discharge from the vagina (with mechanical damage to the mucous membrane, it can be abundant)
- increase in body temperature
Little girls may experience neurotic manifestations: sleep disturbance, increased excitability, tearfulness.
The disease can be acute or chronic. Symptoms of the forms of pathology differ only in the degree of severity.
Diagnosis of kraurosis of the vulva
At the initial stage of the disease, due to the lack of specific symptoms, differential diagnosis of kraurosis with vulvovaginitis, neurodermatitis, vitiligo, leukoplakia, lichen planus and diabetes mellitus is important.
As the disease progresses, the clinical picture of vulvar kraurosis is so pronounced that the doctor makes the diagnosis during a routine gynecological examination.
To assess the degree of changes in the skin and mucous membranes, vulvoscopy is performed, and, if necessary, a microscopic examination of a smear from the cervix for flora, a cytological examination of a smear for atypical cells, an immunogram, and a clinical blood test. If malignancy of the process is suspected, a biopsy of vulvar tissue is prescribed with further histological analysis of the biopsy sample.
Vulvovaginitis: drugs
Local and oral agents are used for treatment.
Vaginal suppositories and creams (Gynex, Clotrimazole, Lomixin) are indicated as local ones. Doctors also prescribe a course of tablet antibiotics (Pancef, etc.). For candidal etiology, antifungal agents are prescribed: Nystatin, Fluconazole, Itraconazole, Metronidazole.
Upon completion of treatment, doctors recommend taking probiotics (Lactozhinal, etc.) to restore the microflora.
If the cause of the disease is worms, anthelmintic drugs are needed: Aldazole, Pirantel.
Preventive measures
It is easier to prevent any disease than to treat it. To prevent vulvovaginitis, the following measures are recommended:
- proper toilet of the vulva. You need to wash from front to back. Do not use products with an aggressive pH environment;
- wearing tailored underwear made from natural materials;
- use of barrier contraception;
- excluding douching without indications - this way you can wash healthy flora;
- visit a gynecologist for consultation 1-2 times a year.
Correction of dry nasal mucosa
Most modern people quite often experience unpleasant sensations characterized as “dryness of the nasal mucosa.” It is expressed in nasal congestion, often alternating, itching, burning, crusting in the nasal cavity, and decreased sense of smell. In addition to the feeling of discomfort, dryness of the nasal mucosa negatively affects the filtration function of the nose - dust particles, bacteria and viruses contained in the air almost freely enter the lungs during breathing.
Various factors can lead to dryness of the nasal mucosa. Quite often, “dry nose” is a side effect of certain medications, primarily antihistamines and drugs containing atropine. The most common is the adverse effects of climate and ecology, staying in rooms with central heating and air conditioning. The humidity of the nasal mucosa is negatively affected by inhalation of hot air, in particular from smoking, rarefied air (during air travel and vacations in the mountains), dust in the air in a number of industries - cement, chemical, etc. In addition, this condition can also be a symptom of a general disease.
The mucous membrane of the nasal cavity is covered with a special ciliated epithelium, consisting of ciliated cells that ensure the transport of mucous secretions (Fig. 1).
Ciliated cells have 250–300 cilia, 7 microns long and 0.3 microns high. Each cilium consists of 9 pairs of microtubules arranged in a ring and surrounding two unpaired central microtubules. The movement of the cilia of the ciliated epithelium of the nasal mucosa is carried out through the sliding of microtubules (Satir P., 1974). Energy for movement is provided by ATP, which is broken down by dynein. Dynein is a Ca/Mg-dependent ATPase. The motor cycle begins with the addition of ATP to the dynein molecule. Cleavage of the phosphate ring during ATP hydrolysis leads to the connection of the dynein molecule and the tubulin molecule of the adjacent outer doublet and is accompanied by conformational changes in the dynein molecule - bending and displacement of the microtubule at a certain distance. This, in turn, causes a new ATP molecule to attach to dynein and break its bonds with tubulin, causing the dynein handle to return to its original shape. The whole cycle is repeated again (Kiselev A.S., Tkachuk I.V., 2006).
The movement of the cilia is strictly directed - from the vestibule of the nasal cavity towards the nasopharynx. Mucociliary clearance is provided by nasal secretions. The source of the secretion covering the epithelium of the nasal cavity is the mucous glands of the nasal mucosa, goblet cells, extravasation from subepithelial capillaries, lacrimal glands, and the secretion of specialized Bowman glands from the olfactory zone of the nose. The volume of nasal secretion in 24 hours ranges from 100 ml to 1–2 liters. The mucous membrane of the posterior two-thirds of the nose is renewed every 10–15 minutes. The function of the cilia is optimal at a temperature of 28–33 °C, a sufficient amount of secretion with a pH of 5.5–6.5. Loss of moisture, a decrease in temperature to 7–10 °C, and an increase in the pH of the secretion to more than 6.5 causes the cilia to stop vibrating.
Elimination of dryness of the nasal mucosa is facilitated by applying an isotonic solution to it. At the same time, the rheological properties of mucus are normalized. It is believed that trace elements contained in an isotonic solution, such as Ca, Fe, K, Mg, Cu, help to increase the motor activity of cilia, activate reparative processes in the cells of the nasal mucosa and normalize the function of its glands. The listed microelements are contained in preparations that are prepared from sea water, sterilizing it and bringing the salt content to isotonic concentration (Otrivin More, Marimer, Aqua Maris, Salin, etc.), and from mineral spring water, which has medicinal properties (salt).
One of the new drugs in this group is Otrivin More, which is a purified, disinfected isotonic solution of ocean water from Brittany, extracted in an ecologically clean area of the Atlantic Ocean, rich in natural microelements. It contains 18 minerals and trace elements.
We examined and treated 50 patients of both sexes aged from 21 to 43 years with complaints of “dry nose” caused by prolonged stay in rooms with dry and/or rarefied air. In the treatment of the main group (25 patients), Otrivin More was used in the form of irrigation of the nasal mucosa 2 times a day for 10 days; in the second (control) group (25 patients), an oil solution of tocopherol acetate and retinol palmitate in the form of drops 2 times a day. The distribution of patients by gender and age, as well as by the severity of clinical manifestations in both groups was comparable. Every three days, the dynamics of the main symptoms were assessed: difficulty in nasal breathing, dryness in the nasal cavity (including the patient’s subjective sensations), the nature and amount of nasal discharge, the state of mucociliary transport (saccharin test).
At the end of the course of treatment, a positive clinical effect was obtained in 42 patients, of which 23 were from the main group and 19 from the control group. In 8 (16%), including 6 from the control group (24%), no positive dynamics were recorded. In the group of patients receiving Otrivin More, the regression of pathological signs was significantly more rapid compared to the control group, which was confirmed by the results of a study of mucociliary transport. On average, the decrease in mucociliary transport time with the use of the drug was 6.9 minutes. In the control group, this figure was 4.3 minutes (Fig. 2).
Changes in mucociliary transport parameters correlated with rhinomanometry data and changes in the clinical picture, which took into account subjective symptoms assessed using a patient questionnaire. The drug was well tolerated by all patients. In addition, all patients noted the ease of use of the drug, while the use of oil drops by the majority of patients in the second group (24 people) was characterized as “inconvenient.”
Thus, Otrivin Sea can be recommended as a means for caring for the nasal cavity not only for patients with rhinitis, including atrophic ones, but also as a means of daily hygienic care for the cavity during the heating season, as well as for people who stay in dry rooms for a long time. and/or rarefied air.
Literature
- Satir P. How cillia move // Scientific American. 1974. Vol. 231. P. 45–46.
- Kiselev A. S., Tkachuk I. V. Spray Aqua Maris for diseases of the nose and paranasal sinuses // Pharmacy Weekly. 2006, March 27, No. 12 (533).
O. V. Zaitseva , Candidate of Medical Sciences, National Research Center of Otorhinolaryngology, Federal Medical and Biological Agency of Russia , Moscow
What complications can there be?
Untreated vulvovaginitis can lead to serious consequences. In girls, the formation of dense adhesions of the labia minora is possible. Such a deformation will make sexual life difficult. In addition, this pathology is one of the factors that provoke cystitis.
The disease is especially dangerous during pregnancy. The expectant mother is at risk of spontaneous abortion, endometritis, or the birth of an infected baby.
Chronic vulvovaginitis leads to hardening of the mucous membranes. With this course, cracks and erosions occur more often, and prerequisites for the appearance of oncology appear.
How does Methyluracil work?
The active component of the drug, when in contact with the surface of the skin or mucous membranes, prevents the development of pathological processes, affects rapidly proliferating cells, favors cellular and humoral immune factors, protects tissues from damage by aggressive substances and radiation, helps fight leukopenia and neuropenia during chemotherapy.
When taken orally, Methyluracil accelerates the healing of erosive damage to the gastrointestinal tract, eliminates inflammatory pathologies, stimulates bone healing in fractures, and restores the normal blood formula. Local forms of the medication help heal non-healing wounds, accelerate recovery from infectious lesions, and prevent secondary infections from occurring during injuries and after surgical treatment.
Popular questions about vulvovaginitis
How to diagnose vulvovaginitis yourself?
The first signs of inflammation are itching, burning and pain in the genital area. These symptoms mean you need laboratory testing to determine the type of pathogen. This is the only way the treatment will be effective.
How often does it occur in children?
Vulvovaginitis occurs quite often in children, because due to age and excessive shyness, girls violate the rules of personal hygiene. In addition, babies often put everything they come across into their mouths, which is why they more often suffer from the helminths that cause this disease.
What complications can there be?
Without treatment, the disease becomes chronic, which can lead to the appearance of an oncological lesion. For girls, there is a high risk of fusion of the labia minora, which is why they may have problems with their sex life in the future.
Prognosis and prevention
How to cure kraurosis of the vulva is unknown. Usually it is not completely cured, but properly selected therapy helps reduce negative symptoms and improve a woman’s quality of life.
Basic clinical recommendations for vulvar kraurosis:
- observe the rules of personal hygiene;
- do not wear synthetic or tight-fitting underwear;
- do not use sanitary pads;
- do not use gels, sprays and deodorants in the intimate area;
- to refuse from bad habits.
The disease requires regular consultations with a gynecologist and ongoing treatment. A properly selected diet and a calm emotional state are of no small importance.