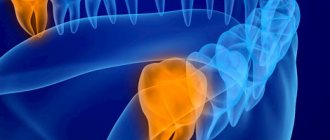
The eruption of wisdom teeth is often accompanied by various complications. This is due to the lack of space in the dentition for the number eight, which erupts last. In dental clinical practice, third molar retention is often encountered - incomplete eruption of the crown above the gum. Removing a wisdom tooth in the gum is a small operation that requires not only extraction of the tooth, but also the creation of access and an incision in the gum. Our dental clinic performs extractions even in the most complex clinical cases. Dentists have extensive experience and high qualifications, and perform procedures painlessly and safely.
A wisdom tooth remains in the gum - is this critical?
Retention or partial eruption is characterized by incomplete emergence of the crown above the gum. Only 1-2 bumps or part of the tooth crown may appear. Retention can be independent or together with dystopia - incorrect positioning of the molar. Symptoms of the disease will depend on the individual clinical situation.
Depending on the location, retention can be vertical, horizontal or angular. With a vertical crown, the tooth crown is located normally in the bone, in accordance with other teeth. Horizontal is characterized by the location of the tooth perpendicular to the others, horizontally to the arch of the jaw. With angular retention, the crown is tilted to the side. According to the depth of its location, the tooth can be covered only by gum, but by a bone plate.
Retention is accompanied by the ingress of food debris and plaque under the gum. This causes inflammation, redness, tissue swelling, and pain. Pericoronaritis may occur - acute inflammation of the gums and mucous hood above the crown of the impacted tooth. The disease can be serous and purulent, causes acute pain, hyperemia, tissue swelling, and makes it difficult to open the mouth.
In most cases, a tooth in the gum is a source of various complications: pericoronitis, the formation of caries and its complications, cysts, stomatitis, periostitis, abscess. Therefore, in case of pathology, dentists recommend removal.
To date, exact methods for preventing retention are unknown. General measures include proper hygienic care of the oral cavity and monitoring the correct development of the child’s jaws and bite. As well as timely and correct orthodontic treatment of malocclusions.
On the top
The most common complication of extraction of figure eights in the upper jaw is a puncture of the base of the maxillary sinus (maxillary sinus).
Puncture of the bottom of the maxillary sinus
The dental roots of molars number three in the upper jaw are located too close to the base of the sinus, and sometimes even grow into it. Chronic inflammation of the periapical tissue provokes resorption of the axillary septum, due to which the roots of the molars fuse with the mucous membrane inside the sinus. It is this part that most often ruptures during the extraction of the right or left tooth. This complication can be noticed by the following symptoms:
- nasal sound, bleeding air bubbles;
- blood from the nose on the side of the figure eight.
In such a situation, urgent medical assistance is necessary.
Indications for removal
Retention can manifest itself as a stage of eruption. Over time, the crown completely appears above the gum and the tooth can function normally. Therefore, the decision on the need for removal should be made by a doctor only after examining and diagnosing the condition of the dental system. Indications for surgery are the following clinical cases:
- Constant pain;
- Complications of eruption;
- Trauma to an adjacent molar;
- Pressure on the dentition and its deformation;
- Horizontal or angular position of the third molar in the jaw;
- Dental crowding, which can be aggravated by wisdom teeth;
- Orthodontic and orthopedic indications, that is, the need for extraction to correct the bite or prosthetics.
Content:
- Peculiarities
- Indications
- Contraindications
- Operation
- Removal methods
- Difficult removal
- Stages
- Diagnostic value
- Does it hurt to remove
- Possible complications
Wisdom teeth or “eight” teeth, located at the edges of the jaw, erupt much later than their counterparts. Moreover, this often happens in adulthood, causing a person many unpleasant moments. The fact is that the structure of the human jaw does not provide enough free space to comfortably accommodate an additional pair of teeth. Therefore, “eights” often put pressure on “sevens”, they grow at an angle, their roots become curved, and it can be difficult to provide them with proper hygienic care, as a result of which caries develops. The peculiarities of the location do not allow for high-quality treatment of the wisdom tooth, and the optimal solution is its removal, since it bears neither a functional nor an aesthetic load.
The process of removing a wisdom tooth in the gum
The removal operation consists of the following steps:
- Preparation. To reduce the risk of postoperative deposits, sanitation of the oral cavity and professional hygiene are carried out with the removal of dental deposits. Elimination of pathological microorganisms and foci of infection promotes rapid wound healing without complications.
- Anesthesia. Before the operation, local anesthesia is performed using a carpule syringe and modern painkillers. The anesthetic is selected for each individual, taking into account individual sensitivity, age, and medical history.
- Creating access to the tooth. In case of retention, the dentist must provide good access so that the forceps can be securely fixed. To do this, size the gums and, if necessary, remove the bone and gingival hood.
- Extraction. The difficulty of molar removal depends on the type of retention and the individual situation. The tooth is fixed with forceps and dislocated; if necessary, additional instruments are used.
- Procedures after removal. After extraction, the tooth socket is inspected and bone fragments and protrusions are removed. The doctor applies a gauze pad and, if necessary, medications to stop bleeding. Sutures are placed on the gum to speed up healing.
- After surgery, the patient is given instructions, advice, and recommendations in the postoperative period.
What drugs are used for pain relief
Just a few decades ago, the only painkiller used by dentists was novocaine. Despite its low toxicity, it very often caused serious complications in patients: from an allergic reaction to anaphylactic shock.
The next step was the use of lidocaine. It is still used to this day in budget dental offices, and has an undeniable advantage: allergies to the drug occur extremely rarely. The problem is different: to prolong the effect of lidocaine, the dentist has to add a drop of adrenaline to it. Moreover, this is done “by eye”. And as soon as the doctor’s hand trembles a little, the patient is guaranteed such unpleasant symptoms as rapid heartbeat and dizziness.
It is much more comfortable for both the doctor and the patient of the dental clinic to deal with articaine anesthetics. These include:
- ubistezin;
- ultracaine;
- septanest.
Firstly, such drugs are administered with a carpule syringe, which ensures that the injection itself is less painful. Secondly, the ratio of adrenaline and anesthetic in the drugs is adjusted to the nearest milliliter. This means that wisdom tooth removal will be painless, and the patient will not experience any side effects.
Important! If the patient is at risk, it is recommended to use an anesthetic that does not contain adrenaline.
Prevention after surgery
The rehabilitation period after removal of an impacted wisdom tooth lasts longer than after a normal one. Healing of the gum socket can take up to 2-3 weeks. During this period, it is important to follow the doctor's recommendations to prevent complications. It is necessary to carefully but delicately carry out hygienic care of the oral cavity. For the first days after the intervention, take painkillers and follow a gentle diet. Too hard, burning foods can damage the gums and cause tissue inflammation.
Dentists also recommend rinsing the mouth after each meal using antiseptic solutions, herbal decoctions, or just water. During the week, you must avoid physical activity, visiting the gym, baths, saunas. If any complications occur, you should not self-medicate; you must immediately seek help from a doctor.
If it hurts, what should you do?
In case of acute pain in the area of the impacted tooth or after extraction, you can take an anesthetic. For this purpose, non-steroidal anti-inflammatory drugs are best suited - Nimessil, Ibuprofen, Paracetamol, Ketanov. At home, you can also carry out hygienic cleaning and rinsing the mouth with antiseptics. For a professional examination and treatment, you must visit a dentist.
On the lower jaw
Standard and non-standard complications after pulling out figure eights on the lower jaw occur more often than on the upper jaw. The lower jaw has a number of features, and there are many obstacles in the area where the wisdom teeth are located.
Nerve damage
The mandibular and lingual nerves are at risk of injury, since they pass close to the wisdom tooth. Such damage causes paresthesia, which is manifested by impaired sensitivity:
- sensory;
- painful;
- taste;
- temperature
In the most severe cases, nerve damage negatively affects vision, hearing, and also provokes paralysis. Patients compare paresthesia with numbness of the jaw in the area of the removed molar. In most cases, this complication disappears on its own within a few days, but sometimes additional drug treatment is required.
Alveolar ridge fracture
A fracture of the alveolar process of the lower jaw occurs when the dentist does not grip the jaw correctly and applies more force than necessary. This is an unlikely complication as the mandible is quite strong. Treatment is carried out under conduction anesthesia and involves repositioning and fixing the fragment in the correct position.
Jaw damage
snapshot of the jaw
Jaw injuries (dislocations and even fractures) also often occur due to the fault of the doctor if the tooth is pulled out too intensely or abruptly. During surgery, it is necessary to remove a significant amount of lower jaw bone to provide access to the problematic molar. Because of this, the sections of the jaw are weakened, which increases the risk of fracture if excessive force is applied. A crack or fracture does not always appear immediately. It happens that the patient notices the first symptoms in the form of pain, swelling, and impaired mobility already at home. Sometimes it takes a week before they appear. Statistics show that jaw injuries during medical procedures account for no more than 0.2% of all jaw fractures.
Soft tissue injuries
By pulling out a molar, the doctor can injure the soft tissues surrounding the molar. We are talking not only about the gums, but also about the cheek, tongue, lips. Injuries are caused by dental instruments (scalpel, drill, forceps). The lip is also often injured by the thread used to suture the gums. This happens due to the carelessness of the doctor or the restlessness of the patient. To avoid complications, you need to sit quietly in the dental chair and not distract the doctor.
Possible consequences
Pericoronitis of the wisdom tooth in the lower jaw is a rather dangerous disease, ignoring which can lead to very unpleasant consequences.
Possible complications of the disease may be:
- abscesses, phlegmon of the vestibule of the mouth, buccal area;
- periostitis;
- osteomyelitis of the jaw;
- periodontitis;
- ulcerative stomatitis;
- actinomycosis;
- paradental cysts.
In addition, if wisdom tooth pericoronitis affects the lymph nodes, if inflammation develops, the lymphatic system may become a victim of infection.
And, of course, without proper treatment, the disease can become chronic and periodically “harass” the patient with unpleasant symptoms. Inflammation can spread to neighboring healthy teeth. Therefore, in order to avoid complications, treatment of the disease should be carried out as early as possible.
Clinical researches
Repeated clinical studies have proven that the two-component mouth rinse ASEPTA ACTIVE more effectively combats the causes of inflammation and bleeding compared to single-component rinses - it reduces inflammation by 41% and reduces bleeding gums by 43%.
Sources:
- The role of anti-inflammatory rinse in the treatment of periodontal diseases (L.Yu. Orekhova, A.A. Leontyev, S.B. Ulitovsky) L.Yu. OREKHOVA, Doctor of Medical Sciences, Prof., Head of Department; A.A. LEONTIEV, dentist; S.B. ULITOVSKY, Doctor of Medical Sciences, Prof. Department of Therapeutic Dentistry of St. Petersburg State Medical University named after. acad. I. P. Pavlova
- The role of hygiene products in the treatment of periodontal diseases (S.B. Ulitovsky Honored Doctor of the Russian Federation, Honored Dentist StAR Prof., Doctor of Medical Sciences, Department of Preventive Dentistry of Pavlov Pavlov State Medical University, St. Petersburg) S.B. Ulitovsky - Honored Doctor of the Russian Federation, Honored Dentist of StAR, Prof., Doctor of Medical Sciences; E.S. Alekseeva - associate professor, candidate of medical sciences; A.A. Vasyanina - associate professor, candidate of medical sciences; V.A. Grigoriev - Associate Professor, Ph.D.
- The use of drugs from the Asepta line in the complex treatment of inflammatory periodontal diseases (N.V. Berezina E.N. Silantyeva S.M. Krivonos, Kazan State Medical Academy. Kazan.) N.V. BEREZINA, E.N. SILANTIEVA, S.M. KRIVONOS Kazan State Medical Academy
Causes of pericoronitis
The disease most often results from:
- epithelial injuries due to difficult long-term tooth eruption;
- impacted (formed, but not erupted outward) teeth;
- atypically located tooth roots;
- thickening of the gum mucosa;
- accumulation of soft plaque under the hood and, accordingly, infection of tissues;
- reduction in the size of the dental arch, lack of space for teething;
The catalyst for pericoronitis of wisdom teeth is often a source of infection in the oral cavity. Very often the disease is provoked by caries, stomatitis or periodontitis. Sometimes the disease occurs against the background of ignoring the rules of personal hygiene, prolonged stress, hypovitaminosis and other conditions accompanied by decreased immunity.