Alas, some people in our society are susceptible to a bad habit - smoking. We will not describe the dangers of this habit, and provide evidence of how teeth deteriorate from cigarettes. The article is devoted to a more practical issue - when will it be possible to smoke the first cigarette after tooth extraction surgery.
Tooth extraction at the DaVinci aesthetic dentistry clinic is performed using the most modern instruments and preparations. The patient must be given an anesthetic injection so that he does not feel pain during the operation. But still, tooth extraction is an operation. After it, an open wound will appear in the mouth, the size of which depends on the size of the tooth. Sometimes dentists place drainage and stitches in the gum. The wound will prevent you from eating your usual foods for some time, but if the patient follows all the doctor’s recommendations, then no complications will arise, and soon the hole will stop bothering you.
INTRODUCTION
If you have been diagnosed with cancer and continue to smoke or use other tobacco products, you may feel that it is too late to quit or that quitting will not benefit you.
Some people deep down feel guilty that smoking may have led to the development of cancer, so they do not deserve additional help or treatment. HOWEVER, IT IS NEVER TOO LATE TO QUIT SMOKING!
Regardless of whether you have previously had cancer or are one of the newly diagnosed patients, quitting smoking and using other tobacco products is beneficial in any case. It is important not only to stop smoking cigarettes, but also to stop using other forms of tobacco, including cigars, pipes, smokeless tobacco (chewing and snuff), as well as so-called alternative tobacco products, including hookahs and e-cigarettes. None of them are safe.
In many cases, there are benefits to quitting smoking after being diagnosed with cancer:
- You will have the support and encouragement of your doctor, nurses, and other health care professionals involved in your care.
- You will feel like you are doing something good for yourself and your life.
- You will be able to focus all your energy on recovery.
Most people who use tobacco want to stop using it. Although it can be quite difficult, many people succeed. In addition, there are various treatment options and resources to help you achieve your goals. It is always possible to quit smoking, and all health care providers involved in your care can help you do so. Use this information to learn more about the benefits of quitting tobacco use after a cancer diagnosis and to find a list of programs and other resources that can help you achieve this goal.
How does an implant take root in a smoker?
The following factors influence the osseointegration of a smoking patient:
- Burns to the mucous membrane due to regular exposure to hot smoke. This provokes hyperkeratosis, which slows down reparative processes. The gums heal worse, and there is a risk of peri-implantitis.
- The functioning of the salivary glands is disrupted, which leads to chronic drying of the mucous membrane. This affects not only the gums, but also the balance of the oral microflora - the number of harmful microorganisms increases, which ultimately provoke peri-implantitis or inflammation of the gums around the implant. This may lead to failure of the structure.
- Nicotine constricts blood vessels, causing spasms. The speed of blood flow slows down, oxygen reaches the tissues less well, and the injured area receives fewer vitamins and building elements. The implant fuses with the bone less well.
- The immune system weakens - the dental system is exposed to the negative influence of bacteria. As a result, inflammation occurs at the implant site.
BENEFITS OF QUITTING SMOKING
There are many physical and psychological benefits to stopping tobacco use after a cancer diagnosis, including:
- Increased life expectancy
- More chances for successful treatment
- Reduce serious side effects from all cancer treatments, including surgery, chemotherapy and radiation therapy
- Faster recovery after treatment
- Reducing the risk of secondary tumors
- Reducing the risk of infectious complications
- Easy breath
- More energy
- Better quality of life
On the other hand, continued use of tobacco carries the following risks:
- Increased life expectancy;
- Shortening life;
- Less chance of successful effective treatment;
- More complications after surgery associated with disruption of the heart and lungs, slower recovery;
- More side effects from chemotherapy, such as infections, fatigue, heart and lung problems, weight loss;
- Additional side effects from radiation therapy, including dry mouth, mouth ulcers, loss of taste, and bone and soft tissue problems;
- Increased likelihood of relapse (cancer returning after treatment);
- Increased risk of other serious diseases related to heart and lung problems, or a second tumor.
Implantation and smoking
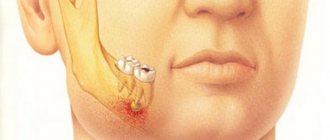
Smoking complicates the operation and increases the likelihood of complications during healing. When a person smokes, thin air is created in the mouth, which prevents the formation of a blood clot. Tissue healing is complicated, and frequent bleeding accompanies the rehabilitation period.
Note: nicotine constricts blood vessels. Because of this, stagnation and suppuration of wounds are formed.
These reasons answer the question: “Why can’t you smoke after having implants installed?” Tissues heal much more slowly than in non-smoking people, osseointegration takes longer. Sometimes smoking after dental implantation causes the sutures placed on the gums to come apart. The risk of implant rejection increases and mobility increases.
Smoking after sinus lift and implantation
Often, before implantation, the dentist prescribes an operation for a smoking patient to increase the bone of the upper jaw, which is otherwise called a sinus lift.
Smoking after bone augmentation surgery or implant installation carries a 10% risk of complications during rehabilitation. The compacted layer of plaque due to tobacco smoke becomes a favorable environment for bacteria and microbes, whose vital activity causes inflammation.
Talking to your doctor about your tobacco use
Many cancer patients are embarrassed to tell their doctor about their habit of smoking or chewing tobacco. They fear that the doctor may judge them or that they may receive less support and assistance from health care providers. Other people think that quitting smoking after being diagnosed with cancer doesn't make sense because they already have cancer and using tobacco can help relieve stress after a scary diagnosis. However, none of these statements are true. There are actually significant health benefits associated with quitting tobacco use, even after cancer has been diagnosed, and the health care providers involved in your care are committed to helping people who want to achieve this goal.
It is important to talk to your doctor or health care provider about your behavior. People who use tobacco products daily have a strong nicotine addiction. This addiction will be difficult to overcome, even if you are motivated to quit. It is necessary to determine the degree of nicotine addiction, which will help the doctor prescribe appropriate treatment. This will help you quit smoking and continue living without dependence on nicotine.
Your doctor needs to know the following facts about your tobacco use:
- Have you smoked at least 100 cigarettes in your life?
- Do you currently smoke
- Do you smoke within the first 30 minutes of waking up?
- How many years and how many cigarettes per day have you smoked regularly?
- At what age did you start smoking?
- How long have you not smoked (if you quit smoking)
- How many times have you tried to quit smoking and how long did each attempt last?
- What methods have you used or are currently using to try to quit smoking?
- Does anyone in your family smoke?
- Do you smoke at work?
- Do you use or have you used other types of tobacco besides cigarettes and how often have you used them?
- Has your tobacco use changed since cancer was diagnosed?
Doctor's recommendations after removal
- 20 minutes after the operation, you need to remove the tampon soaked in antiseptic. During this time, the bleeding should have stopped and the wound should be disinfected. If you leave the tampon in longer, the accumulation of blood and saliva will make it an ideal environment for bacteria to grow.
- A blood clot forms at the wound site, which cannot be picked out and spat out, as it will affect the formation of bone tissue, but for now it will become a natural obstacle to bacteria.
- If you have been prescribed rinses, you need to do them very carefully so as not to wash out the blood clot. It is best to simply draw up the solution, hold it in the desired area for 2-3 minutes and spit. Too vigorous rinsing will damage the clot and slow recovery.
- Sometimes the dentist will apply medication to the socket to speed up healing. They also cannot be removed ahead of time.
- Teeth brushing and rinsing can be done one day after surgery. Only movements with the brush must be careful so as not to remove the blood clot.
- After a complicated wisdom tooth extraction, your dentist may prescribe antibiotics to prevent the infection from spreading. The patient needs to follow the treatment regimen.
- To relieve pain, it is better to apply ice to the cheek; if the pain does not subside, you can take a painkiller.
MYTHS ABOUT SMOKING CESSATION
Myth: Smoking is a completely personal choice.
Fact: In addition to nicotine, tobacco contains addictive chemicals, which is why many people who start smoking quickly become addicted to nicotine.
Myth: There is no point in quitting smoking if cancer is diagnosed.
Fact: It's never too late to quit smoking. People who quit smoking after being diagnosed with cancer live longer, have a better chance of successful treatment, experience fewer side effects from treatment, recover faster and have a better quality of life.
Myth: Quitting smoking is too stressful for patients undergoing cancer treatment.
Fact: Although nicotine addiction is difficult to overcome and quitting can be uncomfortable, the benefits of quitting outweigh any discomfort associated with it.
Myth: Smokers can stop using tobacco on their own without needing a doctor's help.
Fact: Doctors and other health care providers can provide support, information, and medication to help people quit smoking.
Myth: Most tobacco treatment treatments are ineffective.
Fact: There are medications that can help you cope with nicotine addiction and increase your chances of successfully overcoming it. Ask your doctor for help.
results
The study cohort included 52 (14.8%) smoking patients—50 (96.2%) men and 2 (3.8%) women. The age of smoking patients was on average 34.3±1.4 years (from 17 to 55 years). The prevalence of smoking among male 3 kidney transplant recipients was 22% and among females was 1.7%. As a result of the correlation analysis, significant connections between smoking before ATP and the patient’s status after surgery were established ( k
=0.0127;
p
=0.048), as well as transplant status (
k
=0.148;
p
=0.024).
The methodology for assessing survival allowed us to confirm the data of the correlation analysis regarding the effect of smoking on the results of kidney transplantation. The survival rate of smoking patients after ATP was significantly lower ( p
=0.043).
The duration of functioning of transplants in smoking patients was also statistically significantly lower than in non-smoking patients ( p
= 0.038). Data assessing the survival and duration of functioning of the RAT, as well as survival curves are presented in table. 1, 2 and in the figure.
Table 2. Survival rates of RAT patients depending on smoking status before ATP
Survival curves of patients depending on smoking before ATP (a) and survival of RAT patients depending on smoking (b).
1 - survival curve of non-smoking patients; 2—survival curve for smoking patients; 3 — survival curve of RAT of non-smoking patients; 4—survival curve of PAT for smoking patients. In addition to the connections between smoking before ATP and the status of the patient and transplant, statistically significant connections between smoking and other factors were identified: with age ( k
=–0.112;
p
=0.04;
the younger the recipients, the more smokers); gender ( k
=0.389;
p
<0.001; there are more smokers among men than among women);
the period of normalization of creatinine concentration ( k
= 0.140;
p
= 0.016; smoking is associated with delayed normalization of creatinine after ATP);
creatinine level 1 month after ATP ( k
= 0.138;
p
= 0.019) and 6 months after ATP (
k
= 0.143;
p
< 0.022; creatinine level 1 and 6 months after ATP is higher in smoking patients);
development of CTN ( k
=0.274;
p
<0.001);
development of COT ( k
= 0.233;
p
= 0.001) and number of COT (
k
= 0.216;
p
= 0.001; smoking patients have a greater risk of developing COT, and there is also a greater number of them);
Hypertension 6 months after ATP ( k
= 0.148;
p
= 0.05; smoking patients have a higher incidence of hypertension 6 months after ATP);
hemoglobin level 3 months ( k
= 0.129;
p
= 0.044) and 6 months after ATP (
k
= 0.151;
p
< 0.025; smoking patients have a higher hemoglobin level 3 and 6 months after ATP);
albumin level 3 months after ATP ( k
= –0.182;
p
= 0.05; smoking patients have lower albumin levels 3 months after ATP);
alanine aminotransferase (ALT) level before transplantation ( k
= 0.203;
p
= 0.007; smoking patients have a higher ALT level before ATP);
left ventricular hypertrophy (LVH) before ATP ( k
= 0.187;
p
= 0.01; in smoking patients the prevalence of LVH is higher than in non-smokers);
the patient’s willingness to comply with the treatment regimen prescribed by the doctor ( k
= –0.288;
p
<0.001; among smoking patients there are statistically significantly more of those who comply with such a regimen);
return to work after ATP ( k
= –0.168;
p
= 0.02; among patients who smoked before ATP, there were significantly fewer people working after transplantation).
After the operation, only a few smoking patients gave up this bad habit - 42 (12%) patients smoked.
Among 52 patients who smoked before ATP, 36 (69.2%) were alive at the time of the study, 16 (30.8%) died. The mortality structure was as follows: 4 (25%) patients died from infections, 3 (18.8%) from cardiovascular diseases, 5 (31.2%) from other causes, 4 (25%) from unspecified causes. . Among patients who did not smoke before ATP, 147 (81.7%) were alive at the time of the study, 33 (18.3%) died. The structure of mortality among non-smokers was as follows: 14 (42.4%) people died from infections, 7 (21.2%) from cardiovascular diseases, 8 (24.2%) from other causes, and from unspecified causes — 4 (12.1%).
Among patients who smoked before ATP at the time of the study, 23 (44.2%) grafts were lost. At the same time, 11 (47.8%) transplants were lost due to death, due to chronic renal failure - 9 (39.2%), from acute rejection - 2 (8.7%), from other causes - 1 (4.3%). Among patients who did not smoke before ATP, 53 (29.4%) grafts were lost. At the same time, 26 (14.4%) grafts were lost due to death, 21 (11.7%) due to chronic renal failure, 3 (1.7%) due to acute rejection, 1 (0.6%) due to RAT rupture, other reasons - 2 (1.1%). Contingency tables were also used to compare groups of smoking and non-smoking patients by PAT status. As a result, statistically significant differences were obtained in the prevalence of graft losses in the group of smokers ( χ
2=5.08;
p
=0.024). The odds ratio (OR) for PAT loss was 2.05 with a 95% confidence interval (CI) of 1.42 to 2.69.
Among 108 patients with CTN, 72 (66.7%) were non-smokers, 36 (33.3%) were smokers. Among 104 patients without CTN, 93 (89.4%) were non-smokers, 11 (10.6%) were smokers. When comparing these 2 groups, statistically significant differences in the prevalence of CTN were obtained (χ2=15.9; p
<0.001) – high prevalence of CTN among smokers. The OR for the development of CTN was 4.23 with a 95% CI from 3.48 to 4.97.
Among 27 smoking patients with functioning RAT at the time of the study, 19 (70.4%) had CTN, and 8 (29.6%) did not have it. Among 125 non-smoking patients with a functioning RAT at the time of the study, CTN was present in 41 (32.8%) and absent in 84 (67.2%). As a result, statistically significant differences in the prevalence of CTN in the group of smokers ( χ
2=13.1;
p
<0.001). The OR for the development of CTN was 4.87 with a 95% CI from 3.96 to 5.77.
Then, the effect of smoking on the results of ATP was analyzed using multivariate analysis methods. A logistic regression model was built for predicting the outcomes of ATP for the patient's life based on factors associated with the patient before ATP. The analysis included age, gender, BMI, duration of dialysis before ATP, LVH, hemoglobin level, ALT, albumin, the presence or absence of the patient’s work activity during the period of treatment with dialysis, and smoking. As a result, a model was obtained, the main data of which are presented in table. 3. 4 significant prognostic factors for the patient’s life were identified: the level of hemoglobin, albumin, ALT and smoking before ATP.
Table 3. Prediction of the outcome of ATP for the patient's life according to factors associated with the patient's condition before ATP: coefficients of the logistic regression equation
Using logistic regression, a model of the outcome of kidney transplantation, CTN, was built, depending on factors associated with the patient before ATP (Table 4). Two predictors of CTN have been identified: low hemoglobin levels and smoking before transplantation. Low hemoglobin levels and smoking before ATP increase the risk of developing CTN.
Table 4. Prediction of the development of CTN by factors associated with the patient’s condition before ATP: coefficients in the logistic regression equation
A model was also built—transplant status 1 year after ATP based on factors in the pre-transplant period and factors 1 year after ATP. The logistic regression model included the following factors: LVH before ATP, smoking before ATP, levels of hemoglobin, albumin and ALT before surgery, the number of antigenic mismatches according to the HLA system, type of kidney donation (mono- or multi-organ), level of hypertension one year after ATP, levels of creatinine, cholesterol, hemoglobin, proteinuria, albumin in the blood serum 1 year after surgery, as well as patient compliance with the prescribed treatment regimen. As a result of a step-by-step selection of predictors, a model was obtained containing two predictors of ATP outcomes for the patient’s status according to factors 1 year after ATP and factors before ATP: recipient albumin before ATP and recipient smoking before ATP (Table 5).
Table 5. Prediction of the outcome of ATP for the patient's life by factors in the pre-transplant period and factors 1 year after ATP: coefficients in the logistic regression equation
In addition, a Cox model was also constructed for graft status according to pre-transplant factors and factors 1 year after ATP. As a result, a model was obtained (Table 6). This model identified the same predictors of graft ATP outcome: albumin level and pre-transplant smoking.
Table 6. Prediction of outcome of ALT for graft status by factors in the pretransplant period and factors 1 year after ALT: coefficients in the Cox regression equation
HOW TO QUIT SMOKING?
People who want to quit smoking can use a variety of methods, including medication and psychological counseling. Your chances of quitting tobacco use are greatly increased if you use a comprehensive plan that includes: setting a goal date for quitting smoking, developing a plan to deal with smoking triggers (situations that make you want to use tobacco), and creating a “network.” support." Discuss with your doctor which approaches are best for you.
Hookah and cancer risk
One study confirmed that when smoking a hookah for more than 45 minutes, a person inhales the same amount of carbon monoxide as when smoking a pack of cigarettes. Even if the hookah is tobacco-free. An evening in the company of friends smoking increases the level of nicotine in the body, which can cause addiction.
Another danger is toxic chemicals in smoke that cause cancer. Irritation of the mucous membranes of the mouth, larynx and lungs when smoking can develop into inflammation, and then into cancer.
Medications
Using special medications can significantly increase your chances of quitting smoking. There are three types of medications to treat nicotine addiction:
Nicotine replacement therapy (NRT)
NRTs are the most commonly used medications. They have few side effects and are available both over the counter and by prescription in various forms (chewing gum, tablets, skin patch, inhaler, nasal spray).
NRT medications reduce symptoms of nicotine addiction. Your doctor will help you find the best dosage for you based on your current smoking habits.
Bupropion (Wellbutrin, Zyban). These antidepressants can be used to reduce withdrawal symptoms even if you are not depressed. Common side effects include dry mouth and insomnia (difficulty falling or staying asleep).
Varenicline (Chantix). This medication reduces withdrawal symptoms and, if you start smoking again, may reduce the pleasure you get from nicotine. Common side effects - may cause nausea, dreaming, constipation and drowsiness.
Why you can’t ignore discomfort after laser correction
The doctor informs each patient that in the first days, even with strict adherence to all recommendations, slight tearing of the eyes, sensitivity to light, and sensation of a foreign body are possible. There is no need to worry about dilated pupils and slightly swollen eyelids.
Temporary consequences will soon pass, but you should definitely pay attention to obvious discomfort and inform your doctor about the unpleasant sensations. In exceptional cases, an allergic reaction to prescribed medications may occur.
Might also be useful:
- Types of laser vision correction at the Smile Eyes clinic
- Laser correction using LASIK method
Psychological counseling
In addition to the benefits of medications, psychological counseling increases your chances of successfully quitting tobacco use. Discuss with your doctor the possibility of referring you to a smoking cessation counselor or psychotherapist. This is especially helpful if you have been unsuccessful in your attempts to quit smoking or if you experience the following:
- Severe feelings of anxiety or depression
- Insufficient support from family and friends for your desire to quit smoking
- Dependence on alcohol or other substances
Materials and methods
Observational materials from 350 patients who underwent ATP surgery for ESRD were analyzed. The follow-up period after kidney transplantation was 29 years (1985–2014). A total of 229 (65.4%) men and 121 (34.6%) women were observed. The age of the patients was on average 37.1±0.6 years; median age 38 years; minimum 12 years, maximum 61 years.
The main kidney diseases that led to the development of ESRD were chronic glomerulonephritis in 199 (56.9%), chronic tubulointerstitial diseases were observed in 17 (4.9%), congenital kidney diseases, anomalies of the urinary tract - in 23 (6.6% ), diabetic nephropathy - in 11 (3.1%), other nephropathies - in 10 (2.9%) and unspecified nephropathy - in 90 (25.7%) patients.
The average duration of dialysis before ATP was 26.6±1.3 months, the maximum period of dialysis before ATP was 162 months (13.5 years). 342 (97.7%) transplantations were performed using a cadaveric donor, and 8 (2.3%) from living related donors. Three protocols of immunosuppressive therapy were used: 1) cyclosporine + prednisolone + azathioprine; 2) cyclosporine + prednisolone + mycophenolate; 3) tacrolimus + prednisolone + mycophenolate.
The following main outcomes of kidney transplantation were studied: patient status after ATP (alive or not); PAT status (functioning or not); development of chronic transplantation nephropathy (CTN).
At the time of the study, 195 (55.7%) patients remained alive with a functioning graft, 68 (19.4%) lost RAT function and returned to hemodialysis; 87 (24.9%) died. Moreover, 81 (23.1%) patients had CTN at the time of the study. Any loss of PAT (loss of graft function due to rejection or death of a patient with a functioning graft) was considered a loss of PAT. CTN was defined as an increase in serum creatinine concentration of more than 0.13 mmol/L for 3 months or more.
Smoking patients were defined as those who smoked at the time of kidney transplantation. For statistical calculations, the following ATP outcome codes were adopted: for patient status: code 0 - alive, 1 - not alive; for transplant status: code 0 - functioning, 1 - not functioning (lost); for CTN: code 0 - no CTN, 1 - there is CTN.
The analysis used the SPSS application package, version 16. The main statistical methods were descriptive, correlation analysis methods, contingency tables, survival (life tables, Kaplan-Meier analysis), regression analysis (Cox logistic regression). p were considered statistically significant.
<0,05.
Table 1. Patient survival rates depending on smoking status before ATP
Questions for the doctor
Your doctor is your partner in your efforts to quit smoking. You can contact him to get information about the consequences of tobacco use, ways to quit smoking, and other options to achieve your goal.
You can ask your doctor the following questions:
- How does smoking or using tobacco harm my health?
- What are the health benefits of quitting tobacco smoking?
- How does smoking or other tobacco use affect the success of cancer treatment? Will I experience more severe or additional side effects from treatment if I continue to use tobacco?
- What medications are available that can help me quit smoking?
- What behavior or lifestyle changes do I need to make to quit smoking?
- How can I avoid or reduce the triggers that lead to the urge to smoke and use tobacco?
- How can you and your colleagues help me cope with the stress associated with being diagnosed with cancer and quitting smoking?
- What resources are available in my community to quit smoking/tobacco use?
- How can my family and friends help me?
- How often should we discuss the success of quitting tobacco use?
What to do -
Below we will discuss recommended implantation techniques and types of implants for smokers. Below we will talk about two types of implants, which are very different from each other. Firstly, classic traditional implants (in the professional literature they are called “crestal”), which are installed in the spongy bone of the alveolar process of the jaws.
Secondly, about the so-called basal or single-phase implants, which are installed in the deepest layers of the bone. Such implants are safer for smokers in general, and for heavy smokers, they are probably the only reasonable alternative.
When installing classic (crestal) implants –
As we have already said: traditional type implants are installed in the same parts of the bone (cancellous bone) in which the roots of your own teeth are located.
This means that the zone of osseointegration of these implants will begin immediately under the gum mucosa. Thus, the upper part of the osseointegration zone (located around the implant neck) will be almost directly affected by both nicotine and pathogenic bacteria. What to do with all this?
- Firstly – you should choose the right implant model... the success of implantation is largely based on the special properties of the implant surface and, it must be said, that the surfaces of implants from different manufacturers are absolutely not equivalent. As we said above, a history of smoking reduces both the rate of osseointegration and worsens the very quality (strength) of attachment of the implant to the bone.
But there are implant surfaces that have active properties and stimulate osteogenesis on the surface of the implant, which allows, in some way, to compensate for the effects of smoking. The following technologies impart active properties to implant surfaces: the presence of an ultra-hydrophilic surface, surface treatment with fluorine ions, and the presence of a thin layer of phosphorus molecules on the surface of the implant.Implants from the following manufacturers meet these parameters: → AstraTech (OsseoSpeed™ surface), → NobelBiocare (TiUnite® surface), → Straumann (SLActiv® surface), → Osstem (CA surface).
- Secondly – the correct choice of implantation technique... the most important thing you need to remember is that for smokers it is not recommended to use simultaneous implantation with immediate load on the implant (i.e. with immediate or early prosthetics). The choice of this technique will be an almost complete guarantee of its rejection.
It is also not recommended to use a one-stage implantation technique, in which a healing abutment is screwed into the implant at the end of the operation, designed to form a gum contour around the implant already at the stage of osseointegration (Fig. 6). With this technique, although prosthetics are carried out in the long term after surgery, due to the presence of such an abutment, the mucous membrane of the gums will not hermetically seal the implant. The latter means that the bacterial microflora of the oral cavity and nicotine will directly affect the area of osseointegration of the implant.The only reasonable alternative when installing crestal implants in smokers would be to choose the classic two-stage implantation technique, in which the implant is tightly sutured with the mucous membrane immediately after surgery (Fig. 7). Thus, the implant is isolated and pathogenic bacteria will not be able to get to it, and the effect of nicotine will be weakened.
Differences between one-stage and two-stage implantation techniques -
When installing basal (single-phase) implants –
Basal-type implants (Fig. 8) differ from traditional implants in that they are installed in a deeper basal layer of bone. Thus, the working part of the implant (with the help of which its osseointegration with the bone is carried out) is located much deeper from the surface of the mucous membrane than is the case with crestal implants.
As a result, pathogenic bacteria and nicotine have virtually no effect on the osseointegration of the implant. Thus, the incidence of peri-implantitis and implant rejection when using the basal implantation technique is minimized even in smokers (24stoma.ru). Other advantages of this technique are that prosthetics will be possible within 3 days after surgery, and there is no need for bone grafting if there is insufficient bone volume at the implantation site.
It must be said that if you are a heavy smoker, then this type of implant is generally the only option for you. To carry out this implantation technique, implants from two manufacturers can be used, you can familiarize yourself with the characteristics of which, see photos and videos of their use by clicking on the links below:
- ROOTT (Switzerland)
- Ihde Dental (Switzerland)
YOUR PLAN TO QUIT SMOKING
If you are serious about quitting tobacco use, you need to honestly answer the following questions:
- Do you want to quit smoking?
- What is the earliest target date you can set for quitting smoking completely?
- What's stopping you from quitting smoking?
- What fears do you have related to quitting smoking?
- If you've tried to quit smoking before, what made you start smoking again, and what can you change this time?
- How to work with your doctor or other health care provider to create a plan to quit smoking?
- What are your reasons for quitting tobacco use?
You can use the following ideas to get started on creating a quit plan. This plan is not a complete list of recommendations, but just a small list of tips to help you get started.
Why do implants fail?
If smoking occurs after implantation, the patient should be prepared for difficulties and adhere to oral hygiene, more about which you can read here. Structures may be rejected for the following reasons:
- Stone formation on metal pins;
- Acute inflammation of the mucous membrane and gums around the structure;
- Poor blood circulation at the implant site;
- Peri-implantitis;
- Implant mobility and loss.
My Tobacco Quit Plan
- Talk to your doctor, nurse, or other health care professional about different options for quitting tobacco use
- Determine the end date of complete smoking cessation
- Enroll in an in-person or online tobacco cessation program
- Find out about medications that can help you quit smoking
- Seek help to identify and eliminate the factors that push me to use tobacco
Online resources to help quit tobacco use:
- https://kurenie-yad.org/
- https://vrednokurit.ru/
- https://stopsmoking.ru/
- https://www.activestop.ru/
- https://www.legkie.org/
Information prepared based on materials from the American Society of Clinical Oncology* The American Society of Clinical Oncology is the world's leading professional association of oncologists of all subspecialties who treat cancer patients. The organization has more than 30,000 members from the United States and other countries. The society has developed standards of care for cancer patients and is searching for more effective methods of treating cancer, funding clinical and applied research, and, finally, methods of treating various types of cancer, which claims 12 million lives worldwide every year. The ideas and opinions expressed in this information leaflet do not necessarily reflect the views of the American Society of Clinical Oncology or the staff of the Division of Coloproctology and Pelvic Floor Surgery. The information contained in this guide is not a substitute for medical or legal advice. To resolve any issues that arise, the patient should consult a doctor. You should not neglect or delay in seeking professional medical advice based on the information in this information leaflet. Mention of any product, service, or treatment in this guide should not be construed as a recommendation by the American Society of Clinical Oncology or members of the Division of Coloproctology and Pelvic Floor Surgery. The American Society of Clinical Oncology and the Division of Coloproctology and Pelvic Floor Surgery are not responsible for any injury or damage to persons or property, or for any errors or omissions arising from or related to any use of these materials.
Why go to the plastic surgeons of the Pirogov Clinic in St. Petersburg for the best results from mammoplasty?
Plastic surgeons of the clinic named after. N.I. Pirogov has accumulated successful experience in aesthetic and reconstructive breast correction surgeries since 1999. We perform all types of mammoplasty: breast augmentation (endoprosthetics), lift (mastopexy), reduction mammoplasty, correction of gynecomastia, asymmetry and other defects. By contacting us, you can be confident in the high standards of preoperative examination, first-class aesthetic results and the professionalism of our doctors. On our website you can view the portfolio of each plastic surgeon and read reviews about him.
We offer our patients:
- Services of the best plastic surgeons in St. Petersburg, whose professional successes are annually noted by independent experts and industry leaders, as well as by the patients themselves.
- Promotions and special offers (all inclusive) at affordable prices;
- Free face-to-face consultations with plastic surgeons for primary patients.
- Availability of all highly specialized medical specialists whose assistance may be required in one place.
- Our own laboratory, which allows you to quickly obtain accurate diagnostic results - we can send the results of preoperative examinations by email, if that is more convenient for you.
- Operating rooms equipped with new generation medical equipment.
- High comfort and luxury rooms.
- The ability to consult with plastic surgeons remotely using the Online Clinic service.
- Interest-free installment plan for plastic surgery.
- Organizational assistance from a regional manager for patients from other cities.
Conclusion
Oncology doctors carry out a complete diagnosis of the patient. Not only the type and location of cancer is determined, but also its prevalence. Specialists prescribe the optimal treatment method, taking into account the type of cancer and the individual characteristics of the patient’s body. Diagnosis and treatment are carried out using modern equipment. Oncology doctors provide highly qualified consultations that allow them to find answers to many questions of people diagnosed with cancer.
Restriction in food consumption
Dietary nutrition for cancer patients significantly improves treatment results and helps strengthen the human immune system. But speaking of contraindications for cancer, many patients face the problem of poor nutrition. Which foods help restore the body, and which harm it?
Fatty, fried, spicy foods never have a positive effect on the condition of even an absolutely healthy person. Eat in small portions, but often, eat more vegetables and fruits, drink a lot of water - all this will ensure the proper functioning and normal functioning of all internal organs.
Among the most useful vegetables and fruits when diagnosing a malignant tumor, oncology specialists identify beets, broccoli, avocado, basil, nuts, sesame seeds, flaxseed, celery, onions, carrots, fennel, garlic, ginger, pomegranate, blackberries, pears, cinnamon, raspberries , plums, prunes, apples.
Speaking about a number of contraindications for cancer, you should provide a list of foods that are undesirable for consumption:
- carbonated (especially sweet) drinks;
- various bouillon cubes and artificial seasonings;
- soy sauce;
- mayonnaise (excluding homemade mayonnaise);
- fast food products;
- sausages and sausages (excluding home-cooked options);
- products that contain monosodium glutamate and a large amount of vitamin E.
It should be understood that the nature of nutrition plays a significant role in the development of both malignant and benign tumors. Patients diagnosed with cancer are contraindicated from consuming fatty and high-calorie foods, preservatives, smoked, sweet and highly salty foods.
It is worth giving up refined sugar, processed foods, and especially fast food. But patients should increase the amount of protein.
Self-medication and its negative consequences
Non-traditional treatment methods at home are especially dangerous. Under no circumstances should you self-medicate. Acupuncture and manual therapy, cryo- and hirudotherapy, urine and aromatherapy - all this not only does not help, but in some cases worsens the state of health.
Only a competent and comprehensive approach will help achieve positive treatment results. Activities for intensive cleansing of the body are also prohibited. In order not to worsen the situation, you need to contact a specialized clinic.
Hookah and heart and vascular diseases
The smoke that enters the lungs and blood when smoking a hookah negatively affects the body. It is wrong to believe that the water through which smoke passes can cleanse it of toxins.
Why does the heart experience increased stress when smoking a hookah?
- the pulse increases, causing the heart to work harder;
- blood pressure increases, causing the heart muscle to become overstrained;
- the risk of developing a heart attack or stroke increases;
- toxic substances enter the blood, poisoning the internal organs.
Few people consider the hidden health hazards of hookah smoking to be justified. On the contrary, because of the fruity aroma of tobacco, people consider it safe and attractive. Some smokers switch from cigarettes to hookah, believing that they have gotten rid of their addiction. But believing in misconceptions while continuing to smoke means deliberately harming your health.