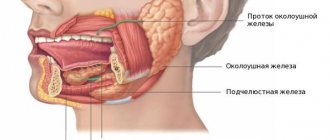
Salivary stone disease is a pathological condition of the body that occurs due to the formation of hard stones in the tissues of the salivary gland. Stones can be located both in the excretory ducts and in the parenchyma of the organ. The disease is predominantly diagnosed in male patients aged 30-50 years. In 90% of clinical cases, stone formation occurs in the submandibular space.
Diagnosis of the disease consists of contrast radiography of the salivary gland ducts, ultrasound examination, study of the biochemical composition of the blood and manual examination of the soft tissues of the maxillofacial area.
Removing a stone from the salivary gland duct is usually not particularly difficult. Until recently, the treatment of stones that were localized in the gland was carried out surgically. During this operation, doctors performed a complete resection of the salivary gland. In Germany, modern clinics offer patients to treat salivary stone disease endoscopically.
Indications for endoscopic removal of salivary gland stones
Removal of stones from the salivary gland is considered a mandatory procedure after a final diagnosis of salivary stone disease has been established. In Germany, the endoscopic technique (sialoscopy) is considered the optimal and effective method of therapy.
Sialoscopy allows you to identify and remove stones in the duct and the gland itself.
Indications
Indications for removal of the submandibular salivary gland are:
- chronic sialadenitis (inflammation);
- benign or malignant tumors;
- multiple cystosis;
- salivary stone disease;
- severe injury to the gland;
- complete blockage of the salivary ducts with the impossibility of restoring their patency.
Depending on the diagnosis, various tests are prescribed before the operation - ultrasound, computed tomography or magnetic resonance imaging, chest x-ray. In the case of a tumor, a biopsy is also necessary to determine the nature of the formation. Salivary stone disease is examined using contrast sialography.
Endoscopic method of treatment of salivary stone disease
Removing stones from the salivary gland without surgery is ineffective. According to modern standards of medical care, this is carried out only with the help of endoscopic intervention. The essence of the technique is to insert an ultra-thin endoscope into the duct of the salivary gland. The diameter of the working part of the tool is 0.9-1.6 mm.
The doctor controls the implementation of such minimally invasive manipulation on the monitor screen. After the specialist has discovered the stone, he uses an endoscope to bring a surgical instrument to the stone to crush and remove it.
Removal of salivary gland stones in Germany is carried out under local anesthesia. The patient is conscious. In some cases, the surgeon may administer premedication, which medically eliminates anxiety, reduces saliva production and enhances the effect of painkillers.
Removing a stone from the duct of the salivary gland or the organ itself in almost 100% of cases leads to a complete recovery of the patient. After such a low-traumatic intervention, the patient experiences a decrease in pain and the disappearance of swelling of the soft tissues of the face.
Performing surgery to remove the salivary gland
With the traditional method of surgery, the patient assumes a lying position with his head thrown back and to the side. The operation involves local infiltration anesthesia. Several parallel incisions are made in the submandibular area, the tissue is lifted, and the capsule of the salivary gland is discovered, which is opened, and the gland tissue is extremely carefully removed and removed. When a malignant tumor grows together with nearby tissues, the latter are also removed. After this, stitches are applied.
During endoscopic surgery, both local and general anesthesia can be used. Through small punctures in the tissue, manipulators and a video probe are inserted, which projects all the actions performed on the screen. When the manipulators reach the gland, small incisions are made with their help, through which pathological tissue is removed. The endoscopes are then removed and sutures are placed at the puncture sites.
Postoperative care of the surgical site includes:
- hygiene - no water or dirt should get into the wounds;
- special diet - the diet will consist of semi-liquid warm food, no hot or cold drinks, no alcohol;
- smoking ban;
- special treatment - it is recommended to regularly treat the seams with antiseptics, and the oral cavity after each meal should be rinsed with a mixture of antiseptic and water.
If all the recommendations of the attending physician are followed, complete wound healing occurs within a few months.
Rehabilitation after removal of salivary gland stones
In the clinic, salivary gland stones are removed by a dental surgeon. After the procedure, he recommends that the patient refrain from eating salty, sour and sweet foods for several days.
It should be noted that after endoscopic intervention there are no special restrictions for the patient. The manipulation lasts 15-20 minutes. At the end of therapy, the patient returns to his normal lifestyle.
In some cases, the doctor may prescribe a course of anti-inflammatory drugs. This measure is a prevention of post-traumatic inflammation of soft tissues in the area of intervention.
What types of stones are there?
Mostly, one particular salivary gland is affected; two are affected at the same time very rarely, all of them are never affected. During the operation, either one stone or multiple stones can occur.
The weight of a stone formed in the salivary gland can reach several tens of grams. In addition, stones differ in their shape. They can be oblong, round or irregular in shape. Very often there are foreign bodies in the center of stones.
Salivary stones consist largely of calcium carbonates and phosphates.
Advantages of endoscopic technology for the treatment of salivary stone disease
Removing a stone from the salivary gland using an endoscope has a number of advantages over traditional surgery. The positive aspects of this treatment are as follows:
- Endoscopic removal of salivary gland stones is performed on an outpatient basis. Thus, patients do not require hospitalization.
- Local anesthesia, which eliminates many complications of general anesthesia. Conduction anesthesia in the treatment of the disease is considered the most effective and safe procedure.
- The low-traumatic nature of the manipulation ensures the integrity of the organ parenchyma and excretory canals.
- Short-term rehabilitation period. After endoscopic intervention, patients do not require a special recovery program or long-term use of anti-inflammatory drugs.
- Complete preservation of organoleptic abilities. Unlike traditional resection, after endoscopic removal of stones, patients retain the ability to perceive sour, salty, spicy and sweet tastes of food.
The price for removing salivary gland stones in Germany depends on the number and size of the stones. The cost of treatment is also affected by the stage of the disease, the general condition of the patient and the presence of concomitant pathologies. Abroad, therapy begins only after a thorough diagnosis and elimination of the inflammatory process in the periglandular tissues.
Specialists of the Deutsche Medizinische Union will offer patients with salivary stone disease as soon as possible to undergo diagnostics in leading German clinics. After the examination, we will organize a consultation with the best specialized surgeon, at which the patient will be familiarized with the final diagnosis, the optimal method of therapy and prices.
DMU specialists are also ready to take upon themselves the organization of travel abroad and the preparation of the necessary medical and legal documentation.
Symptoms indicating inflammation of the salivary glands
The main signs indicating the presence of a stone in the gland duct:
- bursting pain and tingling in the gland area during eating;
- formation of edema in the area of the salivary gland;
- spread of pain to other areas (often the pain radiates to the tongue or throat).
Often, in the place where the stone is located, purulent inflammation of the tissue begins. If the abscess is deep, it can only be seen during surgery or during an examination on an image. If the purulent inflammation is superficial, it will be noticeable to the naked eye.
The presence of stones in the submandibular gland is indicated by the following symptoms:
- dry mouth, causing difficulty chewing food and talking;
- secretion of viscous saliva mixed with mucus and sometimes even pus;
- slow secretion of saliva;
- taste of pus in the mouth;
- swelling of the submandibular area;
- deterioration in general health;
- loss of appetite (pain occurs when eating and the person refuses to eat);
- local increase in temperature.
Symptoms indicating the appearance of stones in the parotid gland:
- a feeling of strong distension in the affected area;
- swelling and redness in the gland area;
- lumbago in the temporal region and ear;
- pain from squeezing;
- dry mucous membranes;
- pain when opening the mouth;
- pus may begin to ooze.
Symptoms indicating stones in the sublingual gland:
- swelling and redness in the mucous membranes;
- the appearance of small nodules at the base of the tongue;
- pain in the cheek area;
- the tip of the tongue becomes painful;
- difficulty swallowing and chewing food;
- in some cases, pus may form and be discharged into the oral cavity.
All these symptoms usually appear and gradually disappear after some time, then return again when eating. The disease develops gradually, and with exacerbation, the accompanying symptoms increase in a matter of hours.
Attention! If you notice similar symptoms described above, immediately visit a dental clinic and consult a specialist.
Results and discussion
In 26 patients, the stones were localized in the middle third of the duct of the submandibular SG, in 17 - in the distal parts of the duct. In all patients, stones were removed using the method described above; in no case was removal of damage to blood vessels or nerves observed. The wounds healed by primary intention without signs of inflammation. Here is a clinical example. The patient had stones removed from the submandibular SG duct using the method described above. Patient P.
appealed to the surgical department of the Central Scientific Research Institute and Maxillofacial Surgery with complaints of swelling in the submandibular region on the right, worsening with food intake.
During a clinical examination, bimanual palpation of the submandibular region revealed a painful round-shaped formation of elastic consistency along the duct of the submandibular fluid on the right. When collecting anamnesis, it was established that patient P.
undergone therapeutic treatment without surgical intervention. However, after some time the symptoms returned.
An X-ray examination of the floor of the mouth revealed stones in the anterior, middle and posterior third of the submandibular duct with a diameter of 0.2 or 0.8 mm.
Removal of stones from the duct of the submandibular gland is a complex surgical procedure that requires a dental surgeon to have good knowledge of the anatomy and topography of the tissues and organs of the oral cavity. In order to prevent possible complications (injury of the lingual nerve and lingual artery) during surgery, it is necessary to isolate the duct of the submandibular SG along its entire length to the calculus, which will allow visualizing the relationship of the lingual nerve and lingual artery and avoiding their damage, especially when removing calculi in the distal part of the duct .
Publications in the media
BENIGN TUMORS . Approximately 80% of parotid tumors are benign. More often they are painless. Many of them are multicentric and often cause local relapses. Very careful identification and surgical treatment are required, consisting of removal of the tumor along with healthy adjacent gland tissue. If it spreads to the deep lobe, a total parotidectomy is performed. During surgery for a benign tumor of the parotid gland, the facial nerve should be preserved.
Mixed tumors consist of both stromal and epithelial cells • Of all neoplasms of the parotid gland they make up 60% • Although they grow slowly, at the time of the initial visit to the doctor they reach a significant size • With enucleation, which during surgery seems easy and radical, leaving is inevitable tumor nests, leading to relapse and the need for repeated intervention • Mixed lesions such as hemangiomas and lymphangiomas are detected in the parotid gland.
Papillary lymphomatous adenocystoma (Warthin's tumor) is found 6 times more often in men aged 40–60 years • Consists of epithelial and lymphoid elements • Tumors (cysts) are soft on palpation • When dissected, a mucus-like substance resembling pus is found inside the tumor. However, despite this appearance, tumors are not inflammatory in origin, but typically neoplastic • Malignant degeneration occurs rarely, mainly in patients who have undergone radiation.
Benign lymphoepithelial tumor (Godwin's tumor) • More often occurs in women of middle age and older • Characterized by slowly progressive lymphoid infiltration of the gland • Malignant lymphoma must be excluded • Rarely, Godwin's tumor does not have a capsule. In such cases, it imitates the inflammatory process • In case of relapses, a good effect can be obtained by irradiation with small doses.
Oxyphilic adenomas consist of acidophilic cells (oncocytes) • They are more often detected in elderly patients • Characterized by slow growth, so the size usually does not exceed 5 cm.
MALIGNANT TUMORS account for 20% of all tumors of the parotid salivary gland. Histological classification: mucoepidermal, mixed tumors, rarely - squamous cell carcinoma, cylindroma, adenocarcinoma.
• Clinic: characteristic symptoms - growth of a tumor-like formation. Characterized by pain and paralysis of the facial nerve, which extremely rarely occurs with benign tumors. The primary diagnosis is established on the basis of clinical examination, palpation, and neurological examination of the cranial nerves. MRI is the method of choice due to the high contrast of soft tissue examination, the ability to determine the growth of the base of the skull, deep tissues of the neck, and base of the tongue. • TNM classification •• T1 - tumor up to 2 cm in greatest dimension without extraparenchymal spread •• T2 - tumor more than 2, but less than 4 cm in greatest dimension without extraparenchymal spread •• T3 - tumor with the following signs: tumor more than 4 , but less than 6 cm in greatest dimension, extraparenchymal spread, but without involvement of the facial nerve •• T4 - tumor more than 6 cm in greatest dimension or extends to the base of the skull, facial nerve • N1 - metastases in one lymph node no more than 3 cm in greatest dimension measurement on the affected side • N2 - metastases in one lymph node on the affected side more than 3 and less than 6 cm in the greatest dimension, or metastases in several lymph nodes on the affected side less than 6 cm in the greatest dimension, or metastases in the lymph nodes of the neck on both sides , or on the opposite side up to 6 cm in greatest dimension.
• Grouping by stage • Stage I: T1–2N0M0 • Stage II: T3N0M0 • Stage III: T1–2N1M0 • Stage IV •• T3N1M0 •• T4N0–1M0 •• T1–4N2–3M0 •• T1–4N0–3M1. • Treatment. The standard of treatment in most institutions is a combination of radiation therapy and surgery.
Low-grade mucoepidermal tumors are usually found in children. In most cases, they are encapsulated and soft on palpation. Treatment is removal of the tumor while preserving the branches of the facial nerve that are not involved in the process. With adequate treatment of low-grade tumors, the 5-year survival rate is 95%.
ICD-10 • C07 Malignant neoplasm of the parotid salivary gland • D11.0 Benign neoplasm of the parotid salivary gland