A panoramic photograph of teeth is often prescribed before and after operations and other complex dental procedures - removal of molars and wisdom teeth, installation of implants, systems for correcting bites, etc. Orthopantomography of the jaws allows you to obtain a three-dimensional image that helps the doctor in treating the patient: prosthetics, restoration integrity of the dentition and other manipulations. The peculiarity of the resulting image is that with its help the specialist immediately observes both the upper and lower rows of teeth, as well as the bone and soft tissue surrounding them.
Equipment for making orthopantomograms
Until recently, analog (or film) orthopantomographs were used to take panoramic images of the jaws. Devices of this type captured the result of scanning the dental system on a special film. The photographs obtained in this way quickly faded, became unclear and were poorly stored.
Today, most dental clinics have digital orthopantomographs, which allow them to obtain higher-quality images, store and send them in digital form, and record them on patients’ electronic medical records. Devices of this type instantly display the results of the studies performed on the monitors of computers connected to them.
In addition, digital orthopantomographs:
- help save time spent on research;
- help reduce the patient’s radiation intensity during the procedure;
- simplify the procedure for deciphering the received images (the doctor can zoom in or out on the image, adjust its contrast, etc.).
What difficulties does radiophobia create during bite correction?
Every sane person who decides to invest substantial funds in correcting a bite with braces wants to get an answer from the dentist to three main questions during preliminary consultations.
- What's wrong with my teeth?
- How can I improve the situation?
- How to save money on braces treatment?
At the same time, the most demanding clients often refuse an X-ray examination: “I will not be exposed to radiation again. It’s enough that they recently forced me to undergo fluorography.”
What should a potential patient of the orthodontist center understand? Locks glued to tooth enamel alone will not correct the bite. The treatment program is developed, activated and controlled by a person. This is a professionally trained specialist who, even before installing metal or aesthetic ceramic braces, must see the goal and imagine the path leading to it.
Teeth can be moved in different ways. The main task that the doctor solves is to choose:
- the correct direction of their movement;
- a device that can do this in the optimal way - effective and most comfortable for the patient.
For this, in-depth diagnostics are performed, and the provider of the most important diagnostic information is precisely the X-ray examination.
Information content of OPTG
An orthopantomogram gives the doctor the opportunity to form a generalized picture of the condition of the masticatory apparatus of a person seeking dental care.
Data obtained from this study help evaluate:
- the correct position of the teeth in the dentition and their location relative to each other;
- general condition of bones in the maxillofacial area;
- quality of previously placed fillings;
- quality of canal filling;
- correct bite formation;
- level of development of tooth roots;
- correct teething (including wisdom teeth);
- the condition of the tissues surrounding the teeth;
- correct position of the dental bones, their shape and general condition;
- correct position of the jaws relative to the sinuses and mandibular nerve;
- symmetry and general condition of the temporomandibular joint;
- effectiveness of dental treatment.
In addition, a high-quality orthopantomogram allows you to identify:
- supernumerary (“extra”) teeth;
- teeth occupying the wrong place in the jaw (dystopic);
- tumor neoplasms;
- cracks and fractures of bones in the maxillofacial area, teeth, dental roots;
- tooth retention;
- carious cavities invisible to the eye;
- cysts, granulomas and other inflammatory foci at the apexes of dental roots;
- periodontal pathology.
What does a panoramic x-ray of the jaw help to identify?
The study is prescribed both for preventive purposes and to identify abnormalities. The most common include:
- damage to the roots of teeth;
- cystic and granulomatous formations;
- various pathologies of the maxillary sinuses;
- inflammatory processes in tissues;
- hidden foci of progressive caries;
- control of the development of impacted (molar) teeth, as well as “eights”.
Sometimes the doctor may advise the child to have an orthopantomography to identify and monitor possible changes in the dental cavity, monitor the rudiments of teeth and their development.
Indications for the procedure
Indications for performing an orthopantomogram are:
- in therapy – the need to draw up a plan for mouth sanitation;
- in orthodontics – diagnosing malocclusions and drawing up a plan for its correction;
- in periodontology – diagnosis of periodontal diseases and drawing up a treatment plan for them;
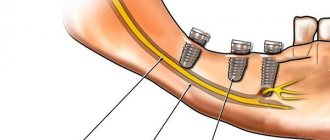
- in orthopedics (including implantology) – planning measures for the installation of prosthetic structures or implantation of dental implants;
- in surgery – assessing the feasibility of surgical interventions (including tooth extraction operations).
Indications and contraindications
Typically, a panoramic x-ray of the jaw is prescribed:
- During the first stages of dental implantation. The image allows you to see the location of hard formations in the oral cavity and calculate the correct location for installing the implant.
- For difficult removal. The image will show how the roots of the tooth are developed, which will simplify and speed up the surgical process.
- For global jaw prosthetics.
- When correcting bites in both children and adults. A three-dimensional image will help you choose the optimal orthodontic system and monitor the movement of teeth during the treatment process.
- In the treatment of periodontal disease and periodontitis to clarify the condition of the tissues.
Contraindications for the study may include pregnancy and breastfeeding. In these cases, the procedure can be prescribed only if emergency intervention is necessary (despite the use of a dose of radiation that is safe for human health during the imaging process). This restriction is especially important to observe in the first trimester of pregnancy.
Procedure for conducting OPTG
OPTG is performed in a specially equipped X-ray room. The procedure consists of a number of stages.
- The patient removes all jewelry (pendants, chains, piercings, earrings, etc.) and removable dentures. The doctor helps him put on a special apron that protects his internal organs from X-ray radiation.
- The patient stands in front of the orthopantomograph and places his chin in a special niche, lowers his shoulders, and straightens his neck. The doctor fixes his head in the correct position using parietal and frontal clamps.
- The doctor turns on the orthopantomograph and an X-ray tube begins to rotate around the head of the person undergoing examination, taking pictures in various projections. A device mounted opposite this tube accumulates x-ray data and transmits it to a computer screen.
- The doctor interprets the orthopantomogram, prints the image or saves it in digital form on a medium.
The total duration of the procedure does not exceed a minute.
Radiation doses during computed tomography
Did you know that the X-ray machine does not have a built-in dosimeter to monitor the radiation dose the patient actually received during the examination?
How then can we find out the radiation dose received during the study?
To assess radiation risks from diagnostic x-ray examinations, there is a characteristic called Radiation AP (DAP). It is defined as the absorbed dose multiplied by the flow area and is expressed in [Gy cm2]. DAP reflects not only the dose in the radiation field, but also the area of irradiated tissue. Therefore, it may be a better indicator of the overall risk of malignancy than simply absorbed dose information. For example, an X-ray machine has several parameters that can be controlled. These are voltage (kV), current (mA), exposure time and irradiation field area. If the input dose is 1 mGy and the field area is 5x5 cm, then the DAP will be 25 mGy cm2. When the field increases to 10 cm x 10 cm with the same input dose, the DAP increases to 100 mGy cm2. This is 4 times higher than the previous value.
Today, medicine is guided by the ALARA principle (abbr. As Low As Reasonably Achievable) - one of the main criteria formulated in 1954 by the International Commission on Radiological Protection in order to minimize the harmful effects of ionizing radiation. This principle involves keeping doses as low as possible and achievably below the limits established by current regulations). Moreover, screening X-ray examinations are prohibited in dentistry. The doctor prescribes a test for the patient only if the risks of not receiving diagnostic information exceed the risks of radiation exposure. Based on the DAP value, the clinician can either reduce the current and voltage to reduce the flow rate, or select a smaller field of view (FOV) to reduce the irradiation area.
So what are the radiation doses received during the study, and what do they depend on?
Information about the DAP level is stored in DICOM files and can be read in the EzDent-i and Ez3D-i programs. More accurate information is provided by dosimetrists when licensing an x-ray room.
What is the radiation dose for OPTG and TRG images?
When using a Vatech PaX-i3D computed tomograph with a field of view of 12x9 cm, the upper limit of the effective dose will be 60 μSv. For a field of 5x5 cm 40 μSv. The upper limit of the panoramic image will be 10 μSv. Cephalometric image (TRG) – 5 µSv. Let's turn to SanPiN 2.6.1.1192-03 and SanPiN 2.6.1.2523-09 to find out the permissible radiation dose per year.
What is the permissible radiation dose per year?
For group A personnel (working directly with sources), the following dose limits are established: On average, 20 mSv per year for any consecutive 5 years. In this case, the annual radiation exposure should not exceed 50 mSv. For Group B personnel (do not directly work with sources, but are exposed to them): On average 5 mSv per year for any consecutive 5 years. In this case, the annual radiation exposure should not exceed 12.5 mSv.
What does the radiation dose depend on?
From the control parameters of the X-ray installation (current strength, voltage, exposure time) and from the irradiation area. And of course, it depends on what tissues and organs were exposed to this irradiation. Some human organs and tissues are more sensitive to the effects of the study than others: for example, at the same equivalent dose, cancer is more likely to occur in the lungs than in the thyroid gland, and irradiation of the gonads is especially dangerous due to the risk of genetic damage. *(1 mSv =1000 μSv)
What is the advantage of digital panoramic dental photography?
- Reduced exposure time, since the digital camera takes less time to create an image. This results in a reduction in radiation exposure to the patient by up to 90%.
- There is no need to develop films, which ensures fast image acquisition, eliminates the need to work with chemicals, and also eliminates the need for repeated x-rays in case of poor-quality development.
- It becomes possible to further examine the resulting images by enlarging individual areas using software.
- Possibility of convenient archiving and quick access to the database with images.
- Immediate transfer to the attending physician located outside the clinic.
- Convenient storage in the form of files.
What images does an orthodontist need?
The standard set required for each patient usually includes:
- orthopantomogram - panoramic photograph of the teeth (OPTG);
- teleroentgenogram - x-ray of the head in profile, and in some cases in front (TRG);
- safe computer scanning of teeth, necessary for diagnostic modeling of the jaws (can be replaced with traditional impression taking);
- and innocuous portrait and intraoral photographs of the patient and his oral cavity.
An orthopantomogram allows dentists of various specializations (therapists, orthodontists, surgeons) to assess the condition of the dental system as a whole, identify wisdom teeth, impacted and supernumerary teeth, the condition of bone tissue, etc. This information is necessary to understand the causes of dental anomalies and develop a corrective program.
A teleradiogram helps a specialist assess his ability to achieve his goal. Not every anomaly can be corrected even with such progressive devices as Smartclip self-ligating braces . In some cases, only surgical intervention can help - at the skeletal level. Using lateral and direct teleroentgenograms, parameters are measured and calculated, the values of which will determine the choice of treatment method. Without such a picture, the result of wearing a brace system can be unpredictable and certainly will not solve the problem.