Chronic periodontitis: description and symptoms
Unlike acute periodontitis, chronic periodontitis is often practically asymptomatic, that is, it is not accompanied by severe swelling and severe pain. That is why many patients come to the doctor when conservative treatment of chronic periodontitis is impossible, and to eliminate complications they have to resort to more radical measures. Chronic periodontitis in the acute stage has much more pronounced symptoms.
Symptoms of chronic periodontitis
- pain
- soft tissue swelling
- tooth mobility
- enlarged lymph nodes
- weakness
- temperature increase
Exacerbation of chronic periodontitis is often associated with concomitant diseases, as well as hypothermia, decreased immunity and other factors.
Symptoms of the disease
General symptoms depend on the form of the pathology. When granulomas form, attacks of pain are observed when exposed to hot food. Pressure on the affected tooth and gum is accompanied by pain. The size and density of the mucosa in the affected area changes, and a granuloma forms under the bone or mucosa.
An exacerbation is accompanied by the appearance of fistulas, which grow and gradually release their contents into the oral cavity. In this case, purulent fistulas can appear not only on the gums, but also on the cheekbones, cheeks, neck, and chin. Isolation of pus may be performed along with the isolation of granulosa tissue. Then the fistula goes away, and a scar appears in its place.
The granulomatous form occurs for a long time without pronounced symptoms. Only after the granuloma grows to a large size and cysts form, the main symptoms appear: discoloration and severe pain in the tooth, development of gumboil and swelling of the gums in the affected area. Cysts that are too large can cause a jaw fracture and long-term rehabilitation.
Fibrous periodontitis is the most hidden form of pathology. There is no pain when chewing food or drinking hot drinks. Severe symptoms are observed only during exacerbation. There is general poisoning of the body due to the penetration of pus into the blood, the tooth becomes loose, and the lymph nodes in this area become larger.
Causes of chronic periodontitis
Chronic apical periodontitis (chronic apical periodontitis, chronic root periodontitis) is so named because the inflammatory process occurs in the area of the apex of the tooth root. This type of disease is often the next stage of the acute form, but it can also develop independently. Based on their origin, experts distinguish two types of chronic periodontitis.
✔
Infectious chronic periodontitis. Occurs as a result of the activity of pathogenic bacteria in the oral cavity. The presence of foci of infection contributes to the penetration of bacteria into periodontal tissue and the development of the disease.
✔
Non-infectious chronic periodontitis. It can be caused by trauma and mechanical damage to the teeth, including due to doctor errors during therapeutic treatment. Another reason may be an allergic reaction to medications (in particular, arsenic and anesthetics), as well as the toxic effects of pulp decay products.
Diagnosis of chronic periodontitis
Unfortunately, without the necessary equipment, it is very difficult to identify chronic periodontitis. A visual examination performs a purely formal function, since even in the presence of symptoms (pain, swelling, etc.), it is necessary to determine the type and stage of periodontitis in order to draw up the most effective treatment plan. Today, diagnosis of the disease is carried out in several proven ways.
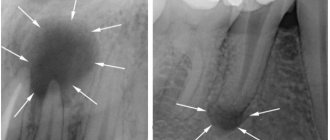
- X-ray examination. The most popular type of diagnostics. All types of chronic periodontitis can most often be detected on a regular targeted X-ray. In case of fistula formation, a narrow-profile X-ray examination - fistulography - is often prescribed.
- Radiovisiographic examination. A more modern and gentle x-ray examination, during which the image is transferred to a computer screen.
- Electroodontodiagnosis (EDD). Diagnosis of inflammatory processes in the dental pulp by monitoring its response to electric current.
- In the case of periodontitis, specialists use differential diagnosis to distinguish it from other dental diseases with similar symptoms.
Chronic forms of periodontitis
Chronic fibrous periodontitis
Periodontal tissues are gradually replaced by connective tissue, and the inflammatory process is usually mild. One of the most common types of periodontitis, which is most often asymptomatic. With exacerbation, pain, enlarged lymph nodes and fever are possible. When diagnosed on an x-ray, you can notice an expansion of the periodontal fissure.
Treatment of chronic fibrous periodontitis is usually easier compared to other forms.
Chronic granulating periodontitis (chronic granular periodontitis)
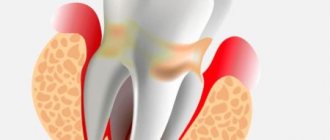
In the apical region of the root, granulation tissue is formed, which actively replaces bone. In terms of symptoms, this is the most pronounced type of chronic periodontitis, which manifests itself in the form of pain, especially when pressing on a tooth or biting. During an exacerbation, the pain intensifies, and fistulas with purulent discharge may occur. On an x-ray, it is quite easy to notice dark, irregularly shaped areas: clear evidence of the development of granulating periodontitis. It is advisable to treat chronic granulating periodontitis quickly enough to avoid the spread of granulation tissue.
Chronic granulomatous periodontitis
A type of periodontitis in which a purulent sac forms near the tip of the root, which, as it grows, first turns into a granuloma, and then into a cyst filled with dense epithelial tissue. The diameter of the cyst can exceed 1 centimeter. In the early stages it hardly manifests itself, but in later stages pain occurs, and the color of the tooth may also change. On x-ray it appears as a dark round spot. Treatment of chronic granulomatous periodontitis in some cases requires surgical intervention, since it is often not possible to get rid of the cyst using conservative methods.
Cyst - what is it and why?
A cyst is a cavity that has an epithelial lining and cystic contents. There are two types of cysts - true and pocket.
The true one is completely covered by the epithelial lining, and the pocket one communicates with the root canal, it seems to grow from it.
Cyst formation occurs in 3 stages.
At the first stage, the epithelial cells of the islets of Malasse most likely proliferate under the influence of growth factors.
During the second stage, an epithelial cavity is formed.
These epithelial cells are directed away from their source of nutrition, die, and neutrophils drag their remains into the area of necrosis. Microcavities are formed, which then merge into one and become limited by stratified squamous epithelium.
There is another theory - the theory that the epithelium covers all open connective tissue areas, resulting in necrosis.
At the third stage of cyst formation after the death of neutrophils, there are reserves of prostaglandins, as well as cytokines produced by macrophages and T lymphocytes. Together they activate osteoclasts and trigger bone resorption.
Pocket cysts have a different mechanism of development. There is a large accumulation of neutrophils near the apical foramen in response to root canal infection. The cells die, as before, and this microabscess is closed by proliferating epithelium. A so-called epithelial ring is formed. Neutrophils that remain outside the channel die and form a microcavity. The presence of infection outside the canal further attracts neutrophils, expanding the microcavity to larger sizes. A pocket cyst is called such because the enlargement of the root canal resembles an enlargement of the periodontal pocket.
Treatment of chronic periodontitis on teeth
Despite the fact that acute and chronic periodontitis are similar in many ways, treatment of chronic forms of periodontitis is usually more difficult and takes longer than the acute form. Treatment of acute chronic periodontitis is most often carried out using conservative methods and may require endodontic intervention: opening the tooth cavity to drain purulent exudate, filling the canals. Antiseptic drugs and antibiotics are also actively used. In the case of chronic periodontitis, the treatment method depends on the stage of the disease and the presence/absence of complications. Based on this, a conservative or surgical treatment plan is drawn up.
Treatment methods for chronic periodontitis
✔
Conservative treatment of chronic periodontitis. It implies a whole range of measures to eliminate the source of the disease. First of all, the tooth canals are cleaned, antiseptic medications are administered, and anti-inflammatory drugs and antibiotics are taken if necessary. After sanitation, the canals are filled with medicinal filling paste, after which it is necessary to wait for the restoration of periodontal tissue for 1 to 3 months. After this period is completed, a permanent filling is performed. In the treatment process, techniques such as electrophoresis, laser and UHF therapy are often used.
✔
Surgical treatment of chronic periodontitis. Surgical methods for treating chronic periodontitis one way or another involve invasive intervention in periodontal tissue. Typically, this technique is used in advanced stages of periodontitis and when complications develop (cysts, fistulas, etc.). Modern dentistry has a number of surgical techniques that allow you to save part of a root or tooth. These include: tooth root resection (removal of part of the root along with a pathological formation), cystectomy (operation to remove cysts and granulomas), and hemisection (removal of the crown part of a multi-rooted tooth along with the root). Despite the fact that chronic periodontitis of permanent teeth is most often tried to be cured with the help of tooth-preserving manipulations, in the most severe cases complete tooth extraction is indicated.
Traumatic periodontitis – Prices
| Services | Price |
| Placing a chemical polymerization filling | 2000 rub. |
| Machining 1 Ni-Ti channel with rotary tools | 1500 rub. |
| Drug treatment of 1 channel | 700 rub. |
| Unsealing of 1 channel, sealed with cement along the entire length | 5000 rub. |
| Unsealing of 1 channel, sealed with cement to 1/3 of the length | 3000 rub. |
| Unsealing of 1 channel, sealed with cement for 2/3 of the length | 4000 rub. |
Make an appointment
Traumatic periodontitis: before and after photos
Repeated treatment of chronic periodontitis
Sometimes specialists have to re-treat chronic periodontitis. This is usually due to the fact that previous treatment was ineffective. This could be poor cleaning and filling of canals, defects during surgical procedures, non-compliance by the patient with rehabilitation rules, as well as an initially incorrectly selected treatment plan. Secondary treatment almost always takes longer and is more difficult. In this case, it is still possible to do without tooth extraction or carry out repeated conservative treatment, however, quite often the patient comes with already developed complications that require surgical intervention.
Chronic periodontitis: treatment at home
Any form of periodontitis cannot be cured at home: this should only be done by a professional doctor. The only option is antibiotic therapy, which in the vast majority of cases is prescribed as an addition to complex treatment. The same applies to traditional medicine. In medical practice, there have been cases when a cyst or granuloma resolved without any intervention, but this should not be attributed to miraculous natural decoctions and tinctures. Much more important are preventive measures that will help improve oral health and avoid problems with teeth and gums. In this case, some traditional medicine can really help, but the main measures to prevent periodontitis are good hygiene, proper nutrition and regular visits to the dentist.
Prevention
Traumatic periodontitis is easier to prevent than to endure pain and risk serious complications. It is necessary to avoid any dental injuries and contact a dentist at the first sign of overload due to improper installation of a filling or orthopedic structure. Those who like to bite thread with their teeth, open bottles, crack nuts, bite a pencil, etc. These habits should be abandoned, especially if the teeth are pulpless. Without a nerve, teeth become more fragile than living ones, and even a small load is enough for chipping to occur at the gum level and traumatic periodontitis developing.