Gingival fibromatosis is the uncontrolled growth of fibrous tissue in the gum and periodontal area. It can be hereditary or acquired, is progressive in nature and requires surgical correction. Without treatment, tissue proliferation will inevitably lead to the development of concomitant pathologies with the formation of periodontal pockets, bone atrophy, loss of healthy teeth and impaired chewing function. Children experience impaired tooth growth and severe malocclusion.
Development factors
The cause of the development of pathological inflammation can be a simple failure to comply with the rules of hygienic care. The condition of soft tissues affects the condition of dentin, since all processes are closely interconnected.
If you notice signs such as redness or swelling, it is recommended to contact your dentist immediately. The causes of inflammation can be general and local in nature.
Common ones include:
- lack of minerals in the body;
- hormonal imbalance;
- bad habits;
- diabetes;
- diseases of the gastrointestinal tract;
- infectious diseases;
- disorders of the cardiovascular organs;
- low immunity;
- long-term treatment with certain groups of medications.
There are also local causes that can increase the risk of inflammation of the mucous membranes of the oral cavity, in particular:
- teething;
- chemical or thermal burns;
- mechanical factors affecting delicate gum tissue;
- dental plaque and tartar;
- non-compliance with the rules for caring for the oral cavity, which leads to the accumulation of pathogenic microbes in periodontal pockets;
- improper implementation of prosthetics.
It is noteworthy that in practice there are cases when the cause of the development of pathology is the sharp edge of the prosthesis or an incorrectly cut filling. In this case, inflammation affects exclusively the site of damage to the mucosa.
How does the disease manifest itself?
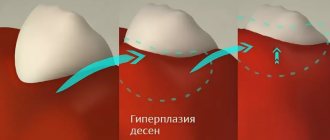
Gum overgrowth affects the outer (buccal) and inner (lingual) areas of the gums, affecting one or both jaws. The general surface of the gums, the gingival margin adjacent to the tooth, as well as the interdental papillae are affected.
Main symptoms of the pathology:
- partial or complete overgrowth of crowns in the area of fibromatosis;
- smooth rounded edge of growths;
- increased density of hypertrophied tissues;
- an even pink tint of the gums and no bleeding.
The intensity of symptoms determines the stage of the disease.
In this case, gum hypertrophy can be generalized or focal. The difference is that if in a focal form only a single lesion is formed, then in a generalized form several pathological areas merge with each other. In severe cases of the disease, fibromatosis can be combined with changes in facial features characteristic of acromegaly.
On a note!
With hereditary pathology, it is impossible to reverse tissue hypertrophy, however, in areas of the gums with extracted teeth, growth usually stops.
Clinical picture
The onset of pathology may be indicated by the appearance of redness and swelling in the affected area. If timely treatment is not started, inflammation spreads to healthy tissue areas, which leads to bleeding, discomfort, and itching.
The gum begins to cover more of the length of the tooth than usual. In the absence of qualified dental care, a change in the shape of the gingival papilla is often observed, and in advanced situations, the gum covers almost half of the element of the dentition.
The listed signs are accompanied by pain, bleeding (especially during and after eating), and a decrease in the quality of chewing function.
Among other characteristic features it is worth highlighting:
- Formation of purulent foci in the space between the teeth.
- The appearance of an unpleasant odor.
- An increase in the volume of soft tissue around the tooth.
- Difficulty eating.
- Uncharacteristic shade of the mucous membrane at the site of the lesion.
- Increased sensitivity.
- Uncharacteristic tissue structure.
In advanced cases, the inflammatory process is complemented by various diseases of the oral cavity, which lead to the destruction of both soft and hard tissues.
Regeneration of the gingival papilla and mucous membrane in the area of the intermediate part of the bridge
Ramon Gomez Meda Doctor of Dentistry, private practice (periodontics and prosthetic dentistry) (Leon, Spain)
Santiago Mareque Bueno Doctor of Dentistry, private practice (periodontology) (Pontevedra, Spain); Associate Professor at the University of Santiago de Compostela
In order for the restoration to look natural and the restored teeth to perform their function correctly, it is necessary to take into account the structure of the gums, the appearance of the lips and the patient’s face as a whole. Mucogingival surgery is used to treat gum recession [1–5].
The interdental gingival papilla is the area of gum between two adjacent teeth. It not only serves as a biological barrier that protects periodontal structures, but also plays a significant role in the formation of the aesthetic appearance. The absence of interdental gingival papillae can lead to problems with pronunciation, as well as the retention of food debris in the interdental spaces [6].
If the interdental gingival papilla is lost, its regeneration is quite difficult. Only a few such cases are known in dental practice [7–14]. However, none of the reports contain information about methods that allow restoration of the gingival papilla [15]. This report describes a surgical method for restoring mucosa and gingival papilla in the pontic pontic area in the presence of bone deficiency.
Surgical technique
The patient, 45 years old, came to the clinic for treatment of periodontal pathology. She complained about the mobility of the two upper central incisors. The patient wanted to restore her appearance and also eliminate periodontal pathology. The central incisors had grade 3 mobility; the pocket depth during probing was 10 mm [11] and 8 mm [21]. In the area of the right lateral incisor, a periodontal pocket with a depth of 10 mm was also found in combination with a vertical bone defect, which indicated a deficiency of bone tissue under the gingival papilla (Fig. 1 a, b).
Rice. 1a. Recession found on the labial side of teeth 11 and 12
Rice. 1b. Recession found on the labial side of teeth 11 and 12
A 7 mm deep pocket was also found in the area of tooth 22.
When collecting anamnesis, no allergies, concomitant diseases or bad habits were revealed. The patient was classified as ASA class 1. Several weeks before surgery, the patient was taught oral hygiene, in addition, subgingival deposits were removed and root surfaces were cleaned. After removal of granulation tissue in the area of the gingival papilla in the area of the 12th tooth, soft tissue recession to a height of 3 mm was discovered. In accordance with Miller's classification, she was assigned class III. On the vestibular side, in the area of teeth 11 and 12, recession of soft tissues to a height of 2 mm was also detected (Fig. 2).
Rice. 2. Vertical defect and class III mobility of teeth 11 and 21
Due to bone loss around the two central incisors, the decision was made to remove them (Fig. 3).
Rice. 3 a - d. The first large connective tissue graft was used in the area of the intermediate part of the bridge to protect the interincisal gingival papilla. We made sure that the temporary prosthesis does not put undue pressure on the graft
When smiling, the patient's gums were partially exposed (no more than a third of the length of the coronal part). At the same time, the color of the gum mucosa was heterogeneous. Photographs, x-rays were taken, alginate impressions were taken and masticography was performed. Based on digital analysis of photographs, diagnostic models were made, which were then placed in the articulator. The patient was then given treatment options. A tooth-supported bridge represents the most current option for replacing missing teeth, especially as an alternative to complex vertical guided bone regeneration, which would require frequent examinations and strict patient compliance. The use of such a prosthesis is less risky than installing an implant-fixed prosthesis if bone and soft tissue are not present in sufficient quantities. The patient had a high sociocultural level and aesthetic preferences. Taking into account other personal factors, in particular the patient’s place of residence, we were forced to choose the fastest, most effective and reliable solution. During her first three visits to the hygienist, the patient cried. Given her emotional instability, we abandoned a comprehensive therapeutic approach to reduce the risk of psychological trauma and possible failure. After the existing problem was explained to the patient, she agreed to remove two central incisors, correct the gums in the area of the intermediate part of the bridge, as well as the gingival papilla using several connective tissue grafts. On the same day, after appropriate preparation of the canines and lateral incisors, a temporary fixed prosthesis was installed. The neck of tooth 12 was prepared accordingly, taking into account the likely future soft tissue reconstruction. Endodontic treatment of the lateral incisors was required. Silicone impressions were made to create a second, more accurate, long-lasting temporary prosthesis and to re-evaluate the case from a biological, functional, and esthetic perspective. Four weeks later, soft tissue recession was detected due to bone resorption on the vestibular side of the maxillary alveolar process.
First, a large connective tissue graft was used (Fig. 4).
Rice. 4 a - d. After the second stage of surgery, the volume of tissue in the area of the right central incisor and the papilla between it and the lateral incisor was increased
Using several soft tissue incisions, a tunnel was created in the area of the pontic pontic (Fig. 4). A 6-0 nylon suture was used to secure the graft. We ensured that the temporary prosthesis did not put undue pressure on the graft (Fig. 4). Then we took a break for 4 months. At the end of the period, an increase in the volume of soft tissues was revealed, which still remained insufficient (Fig. 5).
Rice. 5 a - d. The connective tissue graft was installed using a tunnel approach after frenectomy
We needed more tissue in the area of the right central incisor and the gingival papilla between teeth 11 and 12. The depth of the pocket during probing is 7 mm (Fig. 5). Given the loss of 3-4 mm of papilla tissue, we can conclude that the probable probing depth was 10 mm with a 5 mm bone defect at the level of the papilla. After this, the second phase of surgical intervention began (Fig. 5). The preoperative status of the interdental gingival papilla was determined using the Norland and Tarnow classification [16]. The interdental gingival papilla, vestibular and palatal gingiva were numbed with local anesthesia using 1 capsule of Ultracaine® (articaine HCl/epinephrine, 40/0.005 mg/ml) and 1:100,000 epinephrine solution. For better visualization of the surgical field, a surgical dissecting loupe was used. First, a semicircular incision was made at the mucogingival junction to reposition the labial frenulum (Fig. 6).
Rice. 6 a - d. A diamond cutter was used to remove part of the transplanted epithelium
The second incision was made with a microscalpel from the lost gingival papilla along the gingival sulcus around the neck of the lateral incisor. The blade was turned towards the bone. The incision was made through the entire thickness of the gum tissue and provided access for a mini-curette. The third incision was made along the apical border of the semicircular incision directly towards the bone (Fig. 6). As a result, a gingival-papillary complex was formed. Its mobility was necessary to create free space under the gingival papilla and install a connective tissue graft. In addition, some mobility of the palate tissue was also ensured. The resulting flap was fixed coronally using a curette directed along the gingival sulcus and a small periotome. The amount of donor tissue required was determined during a preoperative assessment of gingival and incisal height in comparison with the expected new location of the gingival papilla. A section of connective tissue of significant size and thickness with a section of epithelium 2 mm wide was taken from the patient’s palate (Fig. 5). An area of epithelium was taken to obtain denser and more fibrous connective tissue, as well as to better fill the space under the coronally fixed tissue flap. The use of a large volume of tissue increased the chances of successful graft engraftment, since the graft was nourished by blood perfusion from a larger area. An area of epithelium was placed on the buccal side of the coronally fixed tissue flap, but was not covered by it (Fig. 6), since epithelium is denser than connective tissue and therefore better suited as a base for the repositioned flap. The connective tissue portion of the graft was placed in the gingival sulcus of the lost gingival papilla to prevent movement of the tissue flap and retraction of the papilla (Fig. 6). A 6-0 nylon suture (interrupted suture) was used to secure the graft in position and stabilize the wound. This microsurgical approach was made possible by using a Zeiss optical microscope. The wound on the palate is closed with a continuous suture. The patient is prescribed amoxicillin (500 mg, three times a day, 10 days), as well as an alcohol-free mouthwash with chlorhexidine (twice a day, 3 weeks). Keratinizing epithelial cells and food debris could be removed from the wound surface using a cotton swab soaked in chlorhexidine gluconate. After 4 weeks, the stitches were removed. The patient was also prohibited from using mechanical means to clean teeth in the wound area for 4 weeks. An earlier examination of the patient was impossible due to the remoteness of her place of residence. The postoperative period passed without complications. The third stage of surgery took place before installation of the permanent prosthesis. Using a diamond cutter, part of the transplanted epithelium was removed (Fig. 7).
Rice. 7 a - c. Transformation of the intermediate part of the bridge after the first and second operations
The area between the pontic and the lateral incisors was not probed for 6 months. As a result of probing, a gingival pocket with a depth of 5 mm was discovered in the area of the lateral incisor, which was only 1 mm greater than the depth of the gingival pocket in the area of tooth 22.
results
The patient's condition was assessed 3 months after the first surgical procedure. Only horizontal tissue growth was achieved in the area of the intermediate part of the bridge (Fig. 8).
Rice. 8 a, b. After the second stage of surgical intervention, the edge of the soft tissue of the gingival papilla was 3-4 mm closer to the incisors than before the operation, while there was no bleeding, and probing did not give negative results
The depth of probing in the area of the lateral incisor before the second operation was 7 mm. A recession of 3 mm in diameter was found in the area of the right lateral incisor (Miller class III). After the second stage of surgical intervention, the edge of the gingival papilla was 3-4 mm closer to the incisors than before the operation. The depth during probing decreased by 4-5 mm. An examination carried out after 2 years showed that the clinical results recorded 3 months after surgery had improved. In particular, there was no black triangle between the artificial crowns of the lateral and central incisor (Fig. 9 a, b).
Rice. 9 a. When checked after two years, no black triangle was found between the lateral and central incisors
Rice. 9 b. When checked after two years, no black triangle was found between the lateral and central incisors
There was no retraction or compression of the papillary tissue, and the probing depth did not increase. Radiographic examination showed improvement in the condition of the underlying bone (Fig. 10).
Rice. 10 a - d. Radiographic examination showed significant improvement in the condition of the underlying bone, although no bone graft was used
The depth of the gingival groove of the papilla is greater than on the opposite side, there is no bleeding, and probing does not give negative results. The success of the procedure depended on the following factors:
- The space between the bone and the coronally fixed gingival papilla was filled with a connective tissue graft.
- The connective tissue was well stabilized by the suture.
conclusions
In clinical cases that present not only a medical but also an aesthetic problem, reconstructive surgery can mask tissue loss, but the patient rarely achieves an ideal appearance. To improve the results of such intervention, periodontal plastic procedures can be used. The use of optics and microsurgical instruments is recommended. This allows the surgeon to improve visibility, avoid unnecessary incisions, and increase the chances of a favorable treatment outcome.
Treatment methods
Treatment tactics are determined taking into account the clinical picture, the degree of development of the disease and other associated factors. Several techniques can be used to eliminate inflammation of the oral cavity.
Anti-inflammatory treatment
To eliminate inflammation, the doctor prescribes antiseptics and pads to the patient. For diagnosed gingivitis, Chlorohexidine (prescribed rinse) or Cholisal (available in gel form) is used.
If the inflammation is associated with periodontitis, the patient is indicated for complex treatment with antibiotics. In the most severe cases, surgery is performed.
To treat pregnant women, the dentist selects gentle medications that are not harmful to the child’s health.
Antibiotic therapy
Antibiotics are prescribed to treat acute forms of gingivitis, as well as diseases caused by pathogenic bacteria. The drug, dosage and course duration are determined by the attending physician. As a rule, antibiotics are prescribed in combination with prebiotics and vitamin complexes.
Surgery
The principle of surgical treatment is to coagulate overgrown gums. The method is widely used in dental practice. The procedure is carried out using a special device with an electrode heated by an electric current.
The technique makes it possible to stop the inflammatory process and eliminate bleeding. After the operation, the gums acquire a normal color, the patient ceases to feel pain and discomfort.
Why does gum fibromatosis occur?
Causes of the disease:
- genetic pathology - single gene mutations, some forms of Down syndrome;
- long-term use of certain medications - antiepileptic drugs, immunosuppressants;
- hormonal disorders – diseases of the endocrine system, long-term use of hormonal contraceptives, anabolic steroids, etc.
Surgery can also provoke tissue proliferation.
In addition, symptoms similar to fibromatosis appear in some types of chronic infectious stomatitis.
A genetically determined form of gum hypertrophy is diagnosed after dental prosthetics and can last a lifetime, requiring periodic treatment. Dosage and hormonal forms can appear regardless of the patient’s gender and age and disappear completely after the cause is eliminated: for example, discontinuation or replacement of the drug, treatment of an endocrine disease.
Properties of hyaluronic acid used in dentistry:
- anti-inflammatory – used for gum inflammation, periodontitis, and dental implantation;
- bacteriostatic – suppresses the growth and development of bacteria in the area of inflammation, which is actively used in the treatment of periodontitis;
- regenerative – helps speed up the healing and recovery processes after surgery;
- improves the fixation of bone materials when used for dental implantation (bone grafting), maintaining the stability and volume of the bone graft;
- restores interdental papillae, reconstructing missing tissues;
- helps in the restoration of tissues inside and outside the joint (injections of hyaluronic acid are used for disorders of the temporomandibular joints), reducing pain, eliminating clicks in the joint and restoring mobility to it.
Let's take a closer look at some areas of application of hyaluronic acid in dentistry.