Cystotomy - one of the surgical methods for treating a cyst formed around a tooth root. The main advantage of this intervention is that the causative tooth is preserved after the operation.
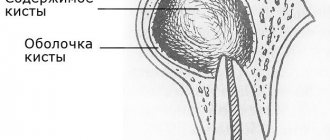
Before choosing a method of treating a cyst, the doctor must send the patient for an X-ray examination. If the image shows that the diameter of the cyst exceeds 8 mm, then conservative treatment will not bring a positive result. It is necessary to choose one of the surgical methods.
More about the operation
Cystectomy is an organ-saving operation that involves complete excision of an ovarian cyst without damaging healthy tissue.
Despite its benign nature, even a small cystic formation can lead to the development of serious complications - dysfunction of the ovaries and menstrual cycle, adhesive disease, infertility. The intervention can be performed as planned or emergency. The second option is used in the development of emergency conditions - rupture of the cyst, torsion of its stem and some other indications. Cystectomy of the cyst is performed laparoscopically, through several micropunctures in the abdominal cavity. The main advantage of this approach is minimal blood loss, low risk of complications and rapid recovery after surgery.
Robot-assisted RC in men
Position of the patient and localization of trocars. The patient is placed in the dorsal lithotomy position, the arms are placed along the body, the lower limbs are spread to the sides so that it is possible to bring the robot. The patient is adequately fixed to the table and placed in the Trendelenburg position at 30-450 (Fig. 1).
Figure 1. Position of the patient on the operating table
After induction of general anesthesia, the surgical field is prepared, a nasogastric tube and a sterile Foley catheter are installed. Correct placement of trocars is very important for the success of the operation. We used a 6-trocar technique with the camera port located 5 cm above the umbilicus in the midline. After insufflation of the abdominal cavity to 10-12 mm Hg. Art. under visual control, two robotic trocars were installed along the navel line on the right and left lateral to the rectus abdominis muscles. The left port is set 8 cm and the right port 10-11 cm from the midline, which provides more space for the assistant's trocar. The third of them is installed 7-10 cm lateral from the left port and 5-7 cm above the iliac crest. When performing intracorporeal urine diversion, this port is replaced with a 15 cm trocar for the stapler, which provides a better angle for resection of the small intestine and the formation of an interintestinal anastomosis. Two assistant ports are located on either side of the right robotic port. The location of the trocars is shown in Fig. 2.
Figure 2. Trocar position
Posterior dissection. Initially, both ureters are mobilized along the lower third from the area of intersection with the iliac vessels to the urinary tract. Closer to the juxtavesical portion of the ureter, two Hem-o-lock clips are applied, between them it is intersected and part of it is sent for pathomorphological examination (Fig. 3).
Figure 3. The left ureter is mobilized along the lower third and clipped
A ligature is applied to the proximal clip, which facilitates further manipulation when anastomosing the ureter with the reservoir. The vas deferens and seminal vesicles are then identified, the wall of the bladder behind the vesicles is mobilized to the Denonvilliers fascia, which is opened, and further dissection is performed between it and the rectum (Fig. 4).
Figure 4. Posterior MP dissection. A) Seminal vesicles. B) Rectum.
Retroprostatic dissection should be performed anterior to the prerectal fat to avoid rectal trauma. If the neurovascular bundles are not preserved, the seminal vesicles are left unchanged on the MP. In the case of nerve-sparing RC, they are allocated closer to the prostate, thereby avoiding damage to the neurovascular bundles, which are located laterally and close to the vesicles.
Mobilization of the bladder and prostate on both sides. After separation of the bladder from the rectum, the bladder is mobilized on both sides. The medial umbilical ligaments are identified closer to the abdominal inguinal ring. The peritoneum is divided laterally to the ligaments extending into the medial portions of the external iliac artery and into the space of Retzii. Using a combination of sharp and blunt dissection, the space between the lateral surface of the bladder and the lateral pelvic wall is widened until the pelvic fascia is reached (Fig. 5).
Figure 5. Excretion of the bladder along the lateral surface to the prostate
In this case, the urachus and umbilical ligaments should not be crossed so that the MP does not fall into the surgical field. The endopelvic fascia is then opened and the lateral surface of the prostate is exposed.
Clipping and intersection of MP vessels. The vas deferens is divided to provide access medial to the external iliac vessels, and lateral dissection is continued. Using the fourth arm, the MP is retracted cranially. With sufficient retraction, the lateral crura can be well identified for division with LigaSure or clipping with Hem-o-lock clips. First, the superior cystic artery is isolated and clipped (Fig. 6).
Figure 6. Clipping of cystic vessels
Next, the inferior cystic and vesicoprostatic arteries are mobilized. Isolation of the pedicles of the bladder ends on the superolateral portion of the prostate near the seminal vesicles while preserving the neurovascular bundles. They are located in the posterolateral part of the prostate and are easily distinguished all the way to the apex of the prostate. Nerve-sparing dissection for RC can be performed using a similar technique as for robot-assisted prostatectomy. The incision is performed in the periprostatic fascia and continues distally to the apex of the prostate. In this case, thermal injury or excessive traction of the neurovascular bundles should be avoided. Next, the vascular pedicles of the prostate are isolated and dissected between Hem-o-lock clips. This technique effectively preserves the lateral periprostatic fascia. We performed infrafascial dissection in patients with low prostate-specific antigen levels, and they did not have prostate cancer in our RC series.
Mobilization of the anterior wall of the bladder and urethra. The urachus and medial umbilical ligaments are coagulated with a bipolar dissector and divided. The anterior wall of the bladder and prostate are distinguished. The dorsal venous complex is ligated and divided, and apical dissection of the prostate and urethra is performed along the length (Fig. 7).
Figure 7. Mobilization of the prostate and urethra
Next, the Foley catheter is removed and a Hem-o-lock clip is placed on the urethra closer to the prostate to prevent urine or tumor cells from entering. Alternatively, a similar clip can be applied to the Foley catheter after tightening its balloon, which assists in traction of the bladder with the prostate (Fig. 8).
Figure 8. After cutting off the urethra, a clip is applied to the Foley catheter.
The released drug is placed in an endobag. The pelvis is washed with an antiseptic solution and hemostasis is performed by coagulation or suturing of bleeding vessels. After drainage is established, the drug is removed through the widened wound of one of the ports.
Why surgery is needed
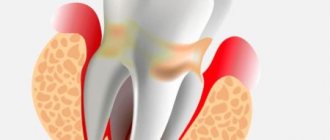
An ovarian cyst is a neoplasm in the form of a cavity filled with fluid. It is not considered a tumor, since in this case completely different formation mechanisms are involved. Small cysts practically do not reveal themselves and do not cause concern, but as the formation grows, or multiple lesions of the ovary (polycystic disease) the functions of the organ are disrupted, which manifests itself:
- disruptions of the menstrual cycle;
- systematic pain in the lower abdomen;
- changes in the nature of menstruation;
- lack of ovulation in the affected ovary, and accordingly the likelihood of infertility;
- intermenstrual bleeding.
The treatment method depends on the examination results and indications. If the cyst does not tend to grow rapidly and does not put pressure on nearby organs, it is treated with medication. In case of multiple lesions of the ovaries, rapid growth of the cyst, severe clinical manifestations, or a non-functional type of cyst, the only effective treatment method is surgical intervention.
Cost of laparoscopic cystectomy
The prices indicated in the price list may differ from the actual prices. Please check the current cost by calling +7 495 104 8605 (24 hours a day) or at the GMS Hospital clinic at the address: Moscow, st. Kalanchevskaya, 45.
| Name | Price |
| Laparoscopic cholecystectomy | RUB 268,800 |
| Laparoscopic cholecystectomy for destructive cholecystitis | RUB 295,680 |
| Laparoscopic cholecystectomy for destructive cholecystitis with peritonitis | RUB 322,560 |
| Laparoscopic cholecystectomy with choledochotomy and drainage of the common bile duct | RUB 349,440 |
| Ovarian cystectomy (ovarian resection) (with laparotomy) | RUB 99,995 |
| Ovarian cystectomy (ovarian resection), bilateral (with laparoscopy) | RUB 145,397 |
| Ovarian cystectomy (ovarian resection), unilateral (with laparoscopy) | RUB 131,397 |
Dear Clients! Each case is individual and the final cost of your treatment can only be found out after an in-person visit to a GMS Hospital doctor. Prices for the most popular services are indicated with a 30% discount, which is valid when paying in cash or by credit card. You can be served under a VHI policy, pay separately for each visit, sign an agreement for an annual medical program, or make a deposit and receive services at a discount. On weekends and holidays, the clinic reserves the right to charge additional payments according to the current price list. Services are provided on the basis of a concluded contract.
Plastic cards MasterCard, VISA, Maestro, MIR are accepted for payment. Contactless payment with Apple Pay, Google Pay and Android Pay cards is also available.
Western standards of treatment (evidence-based medicine)
Continuous staff development
Regular interaction with leading Russian and foreign medical institutions
Modern medical equipment and advanced diagnostic and treatment methods
Unified standard of service
We work around the clock 24/7/365
Make an appointment We will be happy to answer any questions Coordinator Oksana
Discussion
Robot-assisted RC is gradually taking its place in the surgical treatment of patients with muscle-invasive bladder cancer. Robot-assisted access makes it possible to reduce the number of intra- and postoperative complications, primarily to reduce the amount of blood loss, shorten the length of hospitalization and rehabilitation of patients 5, 8, 10, 11. The complexity of RC is aggravated by the comorbidity of patients, who are often elderly. RC is a long-term intervention that includes three defining stages: bladder removal, pelvic lymph node dissection and urine diversion 4, 6, 8. At the beginning of mastering the robot-assisted RC technique, we sought to comparatively simplify the operation, breaking each stage into small steps. When performing them, we tried to follow a certain order of execution, that is, we moved on to each subsequent stage after completing the previous one. There are several key benefits to this structured approach. Firstly, the RC technique is simplified and its results are improved. By working in one specific area, the surgeon's attention was focused on a single task at that time before moving on to the next step. It is important to achieve adequate hemostasis at all stages of RC, which provides good visualization and reduces the amount of blood loss. Even from our initial experience, we were convinced that a systematic approach to performing RC allowed us to reduce the operation time. Secondly, in our opinion, with a detailed description of the individual steps of the operation it is easy to teach young specialists and conduct adequate monitoring of training.
Open RC with extended lymph node dissection remains the gold standard for the treatment of bladder cancer, providing excellent local tumor control with a 50–70% five-year cancer-specific survival rate 13–16. The role of robotic surgery in the treatment of cancer continues to evolve with increasing popularity and is supported by good short- to mid-term results 10, 12, 17. RC is primarily performed for cancer, and therefore the effectiveness of any approach will be judged on the basis of long-term survival outcomes. Robot-assisted RC has been performed in some clinics for more than 15 years; data from robot-assisted RC with Kaplan-Meier analysis were published for 36 and 60 months, comparable to series after open RC 5, 8, 11. Thus, according to Collins JW et al. 8 The five-year cancer-specific survival rate was 67%.
RC through various approaches is associated with a certain number of perioperative complications and severe morbidity 13-16. According to various authors, with open RC their number ranges from 49% to 64% 6, 10, 13-17. Clavien-Dindo high-grade complications range from 13% to 40%, and 90-day mortality range from 0% to 4.5% 13, 16. Robot-assisted RC also has a high complication rate, but relatively fewer, according to compared with open RC 12, 18-20. Collins JW et al. 8 early complications (0-
30 days) was observed in 54 (47.8 %), grade 3 according to Clavien-Dindo - in 37 (32.7 %) patients. Late complications (more than 30 days) occurred in 30 (26.5%), grade 3
according to Clavien-Dindo - in 20 (17.7%), 1 (0.9%) patient died from pulmonary artery embolization. A recent meta-analysis showed that robot-assisted RC compared with open RC is associated with fewer perioperative complications, a higher number of lymph nodes removed, longer operative time, reduced blood loss and fewer blood transfusions, and a short hospital stay. 12 Further prospective studies of robotic outcome -assisted RC with a long period of observation will allow us to confirm the data of this analysis.
What indications to use
Indications for laparoscopic cystectomy are:
- ovarian cyst of small and medium size without signs of malignancy;
- endometrioid, dermoid, mucinous cyst;
- scleropolycystic ovarian disease;
- suppuration of the contents of the cyst;
- the likelihood of cyst rupture or torsion of its stem.
The following symptoms may indicate the presence of an ovarian cyst:
- systematic pain in the lower abdomen, intensifying during menstruation;
- pain during sexual intercourse;
- feeling of “bloating” in the lower abdomen;
- urinary disturbance;
- disorder of the monthly cycle.
The appearance of any of the above signs is a serious reason to contact an experienced gynecologist. You can make an appointment with a specialist by phone or by filling out the feedback form on the website.
Visit to the dentist without pain
Forget the stress of a botched anesthesia, FDC uses painless pain management techniques.
QuickSleeper is an electronic system that provides simple, fast and comfortable pain relief.
VibraJect is a special attachment. It is an effective way to reduce pain and anxiety during local anesthesia. All this helps reduce patient stress from painful injections and unpleasant visits.
Read more about painless anesthesia with QuickSleeper
Preparation, diagnostics
To make an accurate diagnosis and determine the optimal therapeutic regimen, the patient is prescribed a comprehensive examination, including:
- consultation and examination of a gynecologist (vaginal, speculum);
- smears from the cervix and vagina;
- Ultrasound of the uterus and appendages;
- CT, MRI;
- tests for tumor markers (CA-125).
Laparoscopic cystectomy is performed under the following conditions: there is no fluid in the abdominal cavity, tumor markers in the blood do not exceed the permissible norm, and the cystic neoplasm has a homogeneous structure with a smooth surface, clear contours and without foreign inclusions.
The second stage of preoperative preparation involves a standard set of examinations:
- blood tests (for coagulation, infectious group, general, biochemistry) and urine.
- electrocardiogram.
- chest x-ray.
- consultation with a therapist and anesthesiologist.
You should tell your doctor about all medications you are taking, including dietary supplements, existing diseases, previous interventions, drug allergies and other important health facts.
Contraindications
Cystectomy is contraindicated in cases of intolerance to anesthesia and severe concomitant diseases of the heart, liver, kidneys, lungs, blood, diabetes mellitus, exhaustion, and systemic infections. In addition, partial cystectomy is not performed if a reduction in the working volume of the bladder is unacceptable for stage 0 cancer, as well as in cases where the tumor is located near the junction of the ureters and urethra with the bladder (there is no technical ability to ensure urinary function).
How is the operation performed?
Laparoscopic cystectomy is performed under general anesthesia. The operation involves several successive stages:
- The surgeon, through 3 micropunctures, inserts endoscopic instruments equipped with powerful optics into the abdominal cavity.
- To improve visibility of the surgical field, the abdominal cavity is filled with carbon dioxide.
- The doctor uses a clamp to grab and firmly fix the ovary and its ligament, after which he begins to directly remove the cyst.
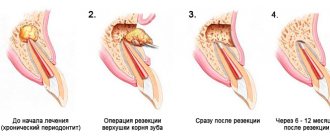
- Using special scissors or a hook, the tumor membrane is cut along the perimeter. If the cyst is more than 8 cm in diameter, first aspiration of its contents is carried out and only after that, the surgeon enucleates the formation and sutures the incision.
The removed tissues and aspirated biomaterial are sent for histological analysis. The intervention can last 30–50 minutes, then the patient is transferred to a hospital, where she remains under the supervision of medical staff for a day.
You have questions? We will be happy to answer any questions Coordinator Tatyana
Materials and methods
On the basis of the Department of Urology of the North-Western State Medical University named after I.I. Mechnikov at the Urology Center with robot-assisted surgery at the Mariinsky Hospital from June to November 2021, robot-assisted RC with intracorporeal orthotopic cystoplasty was performed on 10 patients (8 men, 2 women), age 64-76 years. Body mass index - 25.6±4.5 kg/m2. Preoperative examination included ultrasound examination (US) and spiral computed tomography (SCT) of the abdominal and pelvic organs, SCT of the lungs, and laboratory tests. Bone scans were performed in patients with bone pain or high serum alkaline phosphatase concentrations. Before surgery, all patients underwent urethrocystoscopy, which made it possible to clarify the size and location of the bladder tumor, exclude its presence in the bladder neck (BV) and prostatic urethra, and perform a biopsy for histological verification.
Features of the rehabilitation period
Since the risk of postoperative complications is highest in the first 2 days after the intervention, it is recommended to remain in the hospital during this time. During the first few days, there are minor cramping pains in the lower abdomen, which are easily relieved with conventional analgesics. To avoid complications, a short course of antibacterial and anti-inflammatory therapy is prescribed.
Within a month after the intervention, you must adhere to the following recommendations:
- limit physical activity to moderate - exclude active sports, lifting weights, but you cannot completely limit mobility;
- maintain sexual rest;
- do not visit the bathhouse, sauna, solarium, swimming pool;
- drink enough fluids, follow a diet rich in vitamins and fiber (exclude from the diet foods that cause flatulence and constipation).
To ensure recovery occurs as quickly as possible, physiotherapeutic procedures and other techniques from the arsenal of rehabilitation medicine may be prescribed.
It takes 2.5–3 months for the body to fully recover after removal of an ovarian cyst, after which you need to visit a doctor for a follow-up examination and ultrasound. At the end of the rehabilitation period, you can plan a pregnancy. You can ask all your questions regarding the treatment of ovarian cysts by visiting a gynecologist for a consultation. Doctor appointments at GMS Hospital are carried out by appointment - by phone or online.
results
Robot-assisted RC with intestinal urine diversion was successfully performed in 10 patients. In this work, we considered only the technique of the RC itself. There was no conversion to open intervention. RC time (from installation of trocars to removal of MP) - from 100 to 240 minutes, average time - 120 minutes. The volume of blood loss ranged from 250 to 800 ml (average 370 ml), and, mainly, blood loss was noted at the stage of mobilization of the prostate and dorsal venous complex, its suturing and intersection. Blood transfusion was performed in 3 patients. Postoperative complications were associated with urinary diversion, so we did not consider them in this work. Pathomorphological examination revealed stage pT2 in 6 patients, stage pT3 in 4 patients. Prostate adenocarcinoma was also detected in 3 patients. The removed lymph nodes were negative in all patients.